-
The current coronavirus disease 2019 (COVID-19) pandemic has posed an unprecedented challenge to global health (1-3). The clinical symptoms of COVID-19 are similar to those of malaria, such as fever, myalgia, fatigue, headache, and gastrointestinal symptoms. Due to the heavy burden of medical services and the possible shortage of resources caused by the long-term COVID-19 pandemic, the risk of coinfection of malaria and COVID-19 is a matter of particular concern. Here we reported the first case of COVID-19 coinfection with Plasmodium ovale (P. ovale) malaria in a 47-year-old man who had been previously diagnosed with Plasmodium infection and incompletely treated with antimalarial drugs.
The 47-year-old man worked from October 30, 2018 to December 16, 2020 in Masindi, Uganda, in an area dually affected by malaria and COVID-19. On December 19, 2020, the nasopharyngeal swab for COVID-19 virus testing using reverse transcriptase polymerase chain reaction (RT-PCR) and malaria rapid diagnostic testing (RDT) both had negative results when the patient returned from Uganda and entered Shenzhen City, Guangdong Province, China. However, on December 25, the nasopharyngeal swab for COVID-19 virus test result was positive, and the patient was admitted to a COVID-19 ward for further observation and symptom control on the next day. On December 29, the patient experienced chills, fever, muscle pain, and other clinical symptoms. On December 31, the results of blood smear test showed that the different blood stages of P. ovale, including trophozoites and schizonts, were consistent with P. ovale (Figure 1). In addition, the blood smear identified trophozoites of P. ovale with a parasitemia of 0.01%. The plasmodial ssrRNA (MW768131) and P. ovale sp. tryptophan-rich antigen (potra) (MW872056) gene were amplified by nested PCR, respectively (4-6). After sequencing, the protozoan was identified as P. ovale wallikeri (P. o. wallikeri).
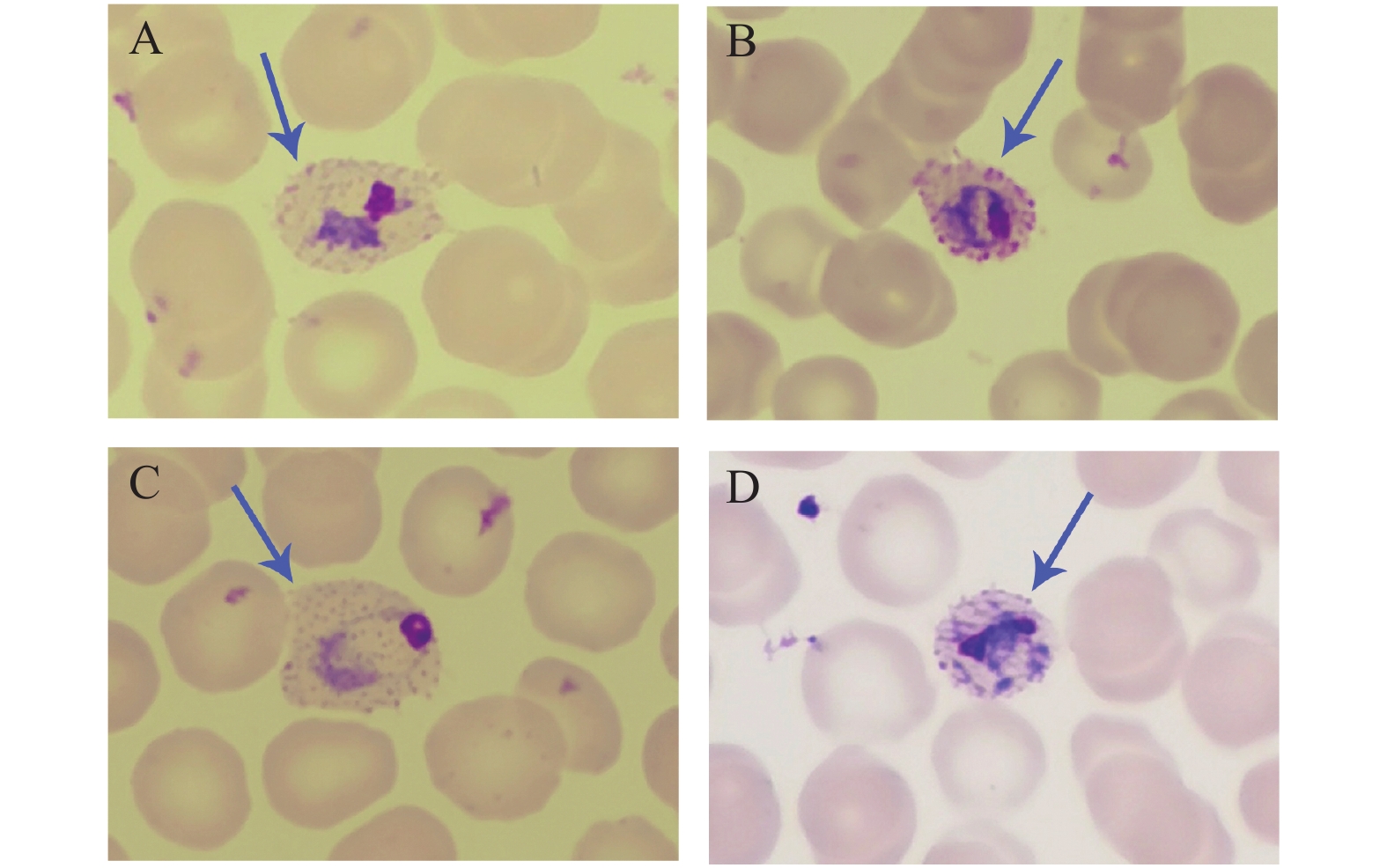 Figure 1.
Figure 1.Giemsa-stained thin blood smears from the peripheral blood of the patient (×1,000). (A) P. ovale trophozoites parasitizing distorted erythrocytes; (B) P. ovale trophozoites parasitizing distorted erythrocytes; (C) P. ovale trophozoites parasitizing enlarged erythrocytes; (D) Early shizont of P. ovale.
The patient’s symptoms were mild and resolved completely after treatment with primaquine for 24 hours. The result of RT-PCR detection of COVID-19 virus swab tested negative on January 1, 2021. During hospitalization, the patient did not have cough, shortness of breath, or other respiratory symptoms including decreased oxygen levels or COVID-19 infection, and did not require any oxygen supply. On January 6, 2021, the blood smear test results were negative for P. ovale. According to his epidemiological history, clinical manifestations, and laboratory test results, this patient was preliminarily identified as an imported case of COVID-19 and P. o. wallikeri malaria coinfection in Uganda.
The patient was recently diagnosed with malaria on December 10, 2020 in Uganda, after which he left this area. During treatment on December 16, there was a possibility of reinfection, which suggested that COVID-19 might induce the current relapse of P. ovale. Similarly, a case of COVID-19 and P. vivax coinfection was reported by Kishore et al., which also highlighted the possibility of COVID-19 infection in inducing current malarial relapse (7). Associated cytokine response with systematic illness has been postulated in P. vivax relapse (8). The COVID-19 infection, with its cytokine response, was assumed to induce the P. ovale relapse of patient. More trials are needed to illustrate the mechanism of COVID-19 in inducing malaria relapse.
During the COVID-19 pandemic, consistent diagnosis of malaria and other infectious diseases should still be prioritized (7,9-11), especially in the areas with endemic infectious diseases such as those in Africa. In addition, invested funds related to malaria elimination were reduced or interrupted and might have lead to the interruption of malaria-related diagnostic tools and drug supply, which might have delayed targets and implementation of the malaria control strategies.
In conclusion, it is necessary to further study the risk factors, clinical outcomes, treatment challenges, and prognosis of cases on COVID-19 coinfection with other pathogens. Given the risk of these diseases, the following comprehensive prevention and control strategies were formulated: 1) 14 days of centralized isolation medical observation for entry personnel in medium and high-risk areas should be implemented, as well as screening for pathogens such as Plasmodium; 2) publicity and education on COVID-19 prevention and control of malaria and other diseases should be continued to reduce the burden of disease or death due to misdiagnosis and missed diagnoses; 3) it is necessary to build human health center communities that supplement existing prevention and control strategies for endemic infectious diseases including COVID-19, malaria, etc. Protecting the health and safety of the global community can only be accomplished with joint effort.
HTML
| Citation: |



 Download:
Download:




