-
“The Clock is Ticking” is the theme of 2021 World Tuberculosis (TB) Day. Each year, we recognize on March 24 the important date in 1882 when the German scientist Dr. Robert Koch announced his discovery of the causes of tuberculosis, that is Mycobacterium tuberculosis, which has caused billions of the death in the past. The fight against TB, one of the threats to global public health, needs to be people-oriented, follow sustainable development principles, and encourage knowledge sharing and policy exchange in the world that was endorsed by the World Health Organization’s (WHO) End-TB Strategy (1–2). In addition, the United Nation (UN) leader’s summit call for further emphasis on TB control and prevention urged the global community to provide treatment to all those with TB in developing countries, to reduce the threat to global public health, and to reduce the economical and labor losses caused by TB (3). World TB Day raises awareness of the challenges that hinder our progress toward the elimination of this devastating disease.
TB is a global disease. In China, TB has been put into category II notifiable disease since 1996. A systematic TB control and prevention program had been launched in the 1990s and has been supported by national effort and prioritization. As a result, TB prevalence in China was halved between 1990 and 2010, mortality rates fell by almost 80%, and incidence rates fell 3.4% per year (4). Despite these achievements, China continues to have one of the highest TB burdens in the world, ranking number 3 in the world in several TB burden indicators.
HTML
-
The Chinese government has been paying close attention to TB control and prevention as the State Council has issued a series of “5-year national TB control programs” (11th, 12th, and 13th) to strengthen the TB control and prevention nationwide and to increase funding for scientific research in terms of diagnostics, digital health, new drugs, new vaccines, and implemental and operational research (5–7). Chinese scientists and specialists continue to carry on investigative studies to understand the burden of TB, the characteristics of the predominant strains (8–10), the effectiveness of infection control measures, means of assisting vulnerable populations, novel drug therapies, and technology to support community case management using mobile phones and medical monitors. The scientific community continues to recognize that TB is impeding the further progress and fulfillment of Healthy China 2030.
Recently, China has established a series of policies and several major measures in its healthcare system, actively and effectively slowed the TB epidemic, and reduced the number of new TB cases by over 300,000 when compared to projections. These are major achievements in TB control and prevention that have had high socioeconomic effectiveness. The central government provided financial support of approximately 1.2 billion CNY for TB control and prevention every year, and local governments and health insurances supplement this figure.
-
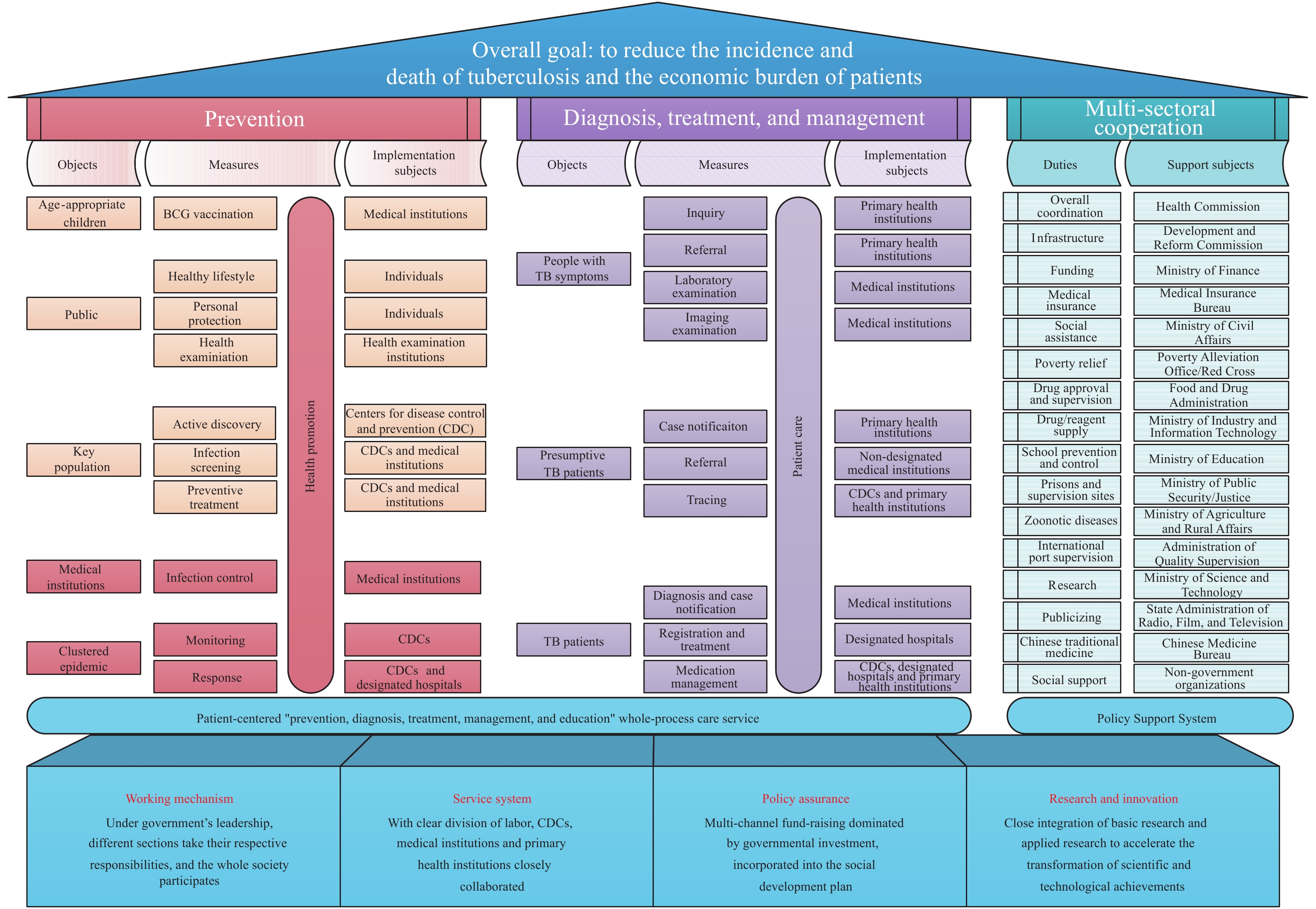
The National TB Program (NTP) is committed to strengthening research on strategies and measures for TB control and prevention; organizing and implementing action plans; conducting scientific research on applying these techniques; providing technical guidance, staff training and quality control for disease control and prevention and public health services throughout the country; and acting as the national technical leading work group for TB prevention and control (Figure 1).
To address these challenges, scientific research and innovation are key to controlling and ultimately eliminating this disease. Innovations in TB control efforts have embraced new tools and approaches to prevent, diagnose, and treat TB and drug-resistant TB (11–15). However, the research is continuous and treating TB depends on multidisciplinary and multisectoral collaboration across the country because the problems are complex and multifaceted and cannot be solved simply. Therefore, international and domestic scientists and stakeholders must collaborate in research and development of new vaccines and new anti-TB drugs.
-
TB is a major priority due to the costs and challenges it brings to the basic public health service system, hierarchical medical system, family doctor signing system, and payment of medical costs by categorizing cases (based on diagnosis-related groups, DRGs). These challenges must be overcome by improving service at the county and township levels by further reforming the healthcare system in conjunction with improving basic health insurance, medical care, medical aid, etc.
China has the capability to act urgently and quickly by partnering with international collaborators. China will, together with international collaborators, harness individual and collective resources under the stewardship by UN and WHO to overcome barriers that impede treatment and address this global challenge (Figure 2).
-
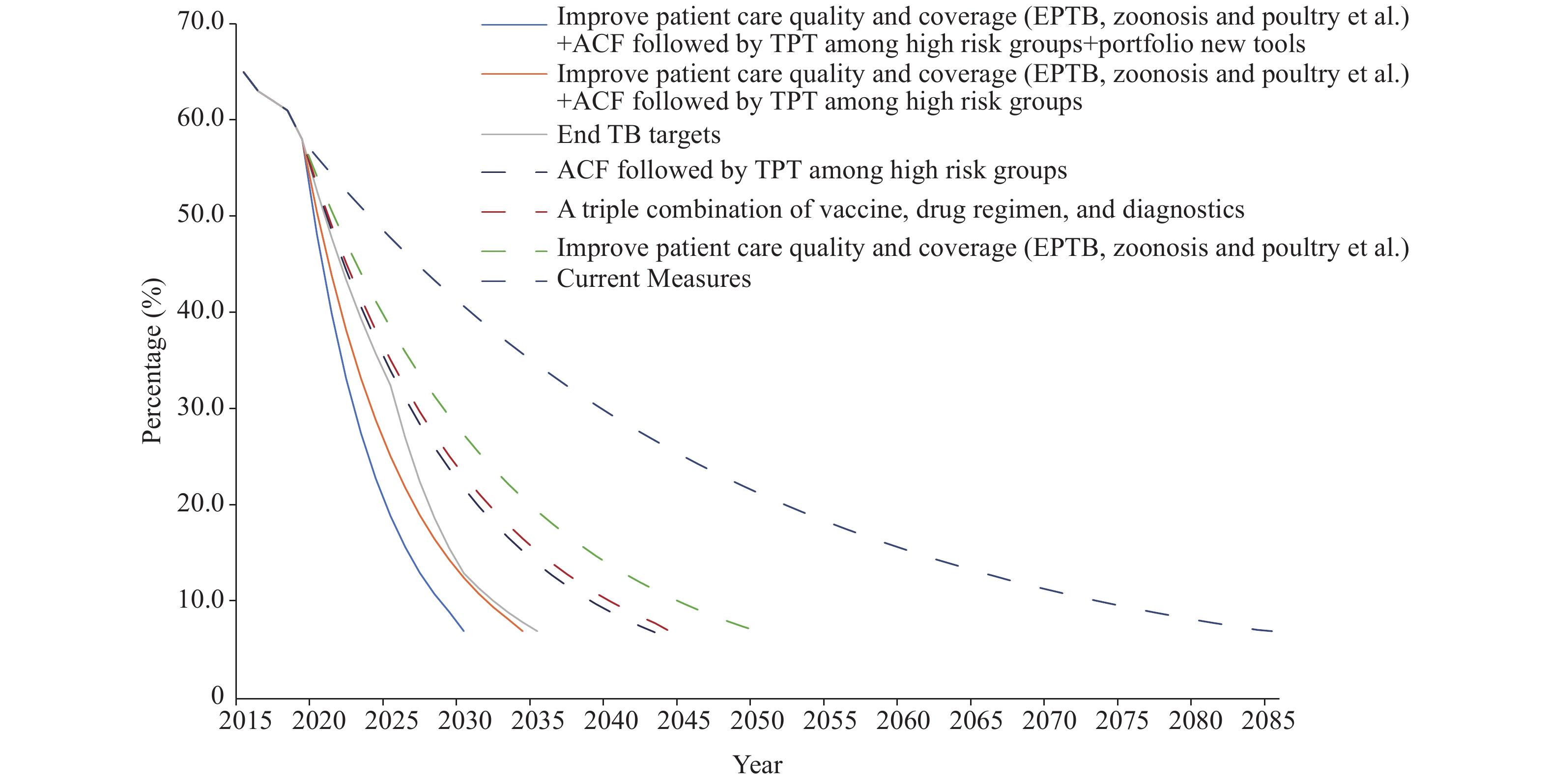
Based on the ambitious targets of the End TB strategy and the baseline TB incidence rate in 2015 (65/100,000 population), the phased indicator of TB incidence rate in China in 2025, 2030, and 2035 was 33/100,000, 13/100,000, and 7/100,000, respectively. The End TB targets are deliberately ambitious, and any single intervention is unlikely to achieve these goals. Policymakers must identify what interventions and at what level of scale up will be needed to meet the End TB targets at the country level. The main interventions including optimizing the use of existing tools enabled by investments in universal health coverage to scale up the active case-finding targets and improve TB preventive treatment among high-risk population to adopt and scale up novel tools (diagnostics, drugs, and vaccines) (Figure 3).
| Citation: |





 Download:
Download: