-
Tuberculosis (TB) is a global public health problem. The World Health Organization (WHO) proposed that the incidence rate of TB should be reduced to less than 55/100,000 population by 2025, less than 10/100,000 by 2035, and to eliminate TB by 2050 (incidence rate <1/100,000) (1). Based on the directly observed treatment, short-course (DOTS) strategy nationwide, China halved the prevalence and mortality of TB in 2010 as compared to 1990 (2), and the cure rate of TB has been reached 92.9% in 2013 (3). The TB incidence rate fell 43.1% from 1990 (130/100,000) to 2010 (74/100,000) (4). Despite impressive achievements, China is still one of the 30 high-TB burden countries in the world. In 2019, there were about 833,000 new TB cases in China with a TB incidence rate of 58/100,000 (4). China also has the highest latent TB infection (LTBI) burden globally with approximately 350 million infections that are at risk for active TB disease (5).
Shanghai is one of the areas with the best implementation of TB control measures in China, but the incidence rate was still above 25/100,000 in 2019 (6). Shanghai failing to reach the target by 2035 would indicate a high likelihood of failure for other areas in China. We established a dynamic TB model to estimate the predicted incidence in Shanghai and the impact of different prevention and control measures.
According to the natural progressive history of pulmonary TB, the overall population was divided into 7 classes: S referred to people who are not infected with Mycobacterium tuberculosis (M. tb); E referred to people infected with M. tb but were not yet infectious; I referred to patients with infectious pulmonary TB; IU1 referred to the undetected and drug sensitive population; IU2 referred to the undetected and rifampicin resistant population; IF1 referred to the detected and drug sensitive population; IF2 refers to the detected and rifampicin resistant population; and R referred to TB patients who have been successfully treated. In this model, we made the following assumptions: 1) the population was evenly mixed, and contact between all individuals was equally likely; 2) patients were likely to infect susceptible population and the recovered after contact with them; 3) all detected pulmonary TB cases were reported to National Notifiable Disease Reporting System; and 4) the total population of the system was relatively stable. The population supplement was due to births in each year, and population loss was due to natural deaths from each group and deaths due to pulmonary TB from patients.
The equations of the model are as follows:
$${\left\{ {\begin{array}{*{20}{l}} {\dfrac{{{\rm{dS}}}}{{{\rm{dt}}}}{\rm{ = \Lambda - }}{{\rm{\beta }}_{\rm{1}}}{\rm{(}}{{\rm{I}}_{{\rm{U1}}}}{\rm{ + }}{{\rm{I}}_{{\rm{F1}}}}{\rm{)S - }}{{\rm{\beta }}_{\rm{2}}}{\rm{(}}{{\rm{I}}_{{\rm{U2}}}}{\rm{ + }}{{\rm{I}}_{{\rm{F2}}}}{\rm{)S - }}{{\rm{\mu }}_{\rm{0}}}{\rm{S}}}\\ {\dfrac{{{\rm{dE}}}}{{{\rm{dt}}}}{\rm{ = }}{{\rm{\beta }}_{\rm{1}}}{\rm{(}}{{\rm{I}}_{{\rm{U1}}}}{\rm{ + }}{{\rm{I}}_{{\rm{F1}}}}{\rm{)S + }}{{\rm{\beta }}_{\rm{2}}}{\rm{(}}{{\rm{I}}_{{\rm{U2}}}}{\rm{ + }}{{\rm{I}}_{{\rm{F2}}}}{\rm{)S - \kappa E - }}{{\rm{\mu }}_{\rm{0}}}{\rm{E}}}\\ {\dfrac{{{\rm{d}}{{\rm{I}}_{{\rm{U1}}}}}}{{{\rm{dt}}}}{\rm{ = \kappa (1 - }}{{\rm{\tau }}_{\rm{1}}}{\rm{)(1 - \sigma )E + \omega (1 - }}{{\rm{\tau }}_{\rm{2}}}{\rm{)(1 - \sigma )R - \rho }}{{\rm{I}}_{{\rm{U1}}}}{\rm{ - \sigma }}{{\rm{I}}_{{\rm{U1}}}}{\rm{ - }}\left( {{{\rm{\mu }}_{\rm{0}}}{\rm{ + }}{{\rm{\mu }}_{\rm{1}}}} \right){{\rm{I}}_{{\rm{U1}}}}}\!\!\!\!\!\!\\ {\dfrac{{{\rm{d}}{{\rm{I}}_{{\rm{U2}}}}}}{{{\rm{dt}}}}{\rm{ = \kappa }}{{\rm{\tau }}_{\rm{1}}}{\rm{(1 - \sigma )E + \omega }}{{\rm{\tau }}_{\rm{2}}}{\rm{(1 - \sigma )R + \rho }}{{\rm{I}}_{{\rm{U1}}}}{\rm{ - \sigma }}{{\rm{I}}_{{\rm{U2}}}}{\rm{ - }}\left( {{{\rm{\mu }}_{\rm{0}}}{\rm{ + }}{{\rm{\mu }}_{\rm{2}}}} \right){{\rm{I}}_{{\rm{U2}}}}}\\ {\dfrac{{{\rm{d}}{{\rm{I}}_{{\rm{F1}}}}}}{{{\rm{dt}}}}{\rm{ = \kappa (1 - }}{{\rm{\tau }}_{\rm{1}}}{\rm{)\sigma E + \omega (1 - }}{{\rm{\tau }}_{\rm{2}}}{\rm{)\sigma R + \sigma }}{{\rm{I}}_{{\rm{U1}}}}{\rm{ - \rho }}{{\rm{I}}_{{\rm{F1}}}}{\rm{ - }}{{\rm{\gamma }}_{\rm{1}}}{{\rm{I}}_{{\rm{F1}}}}{\rm{ - }}\left( {{{\rm{\mu }}_{\rm{0}}}{\rm{ + }}{{\rm{\mu }}_{\rm{1}}}} \right){{\rm{I}}_{{\rm{F1}}}}}\\ {\dfrac{{{\rm{d}}{{\rm{I}}_{{\rm{F2}}}}}}{{{\rm{dt}}}}{\rm{ = \kappa }}{{\rm{\tau }}_{\rm{1}}}{\rm{\sigma E + \omega }}{{\rm{\tau }}_{\rm{2}}}{\rm{\sigma R + \sigma }}{{\rm{I}}_{{\rm{U2}}}}{\rm{ + \rho }}{{\rm{I}}_{{\rm{F1}}}}{\rm{ - }}{{\rm{\gamma }}_{\rm{2}}}{{\rm{I}}_{{\rm{F2}}}}{\rm{ - }}\left( {{{\rm{\mu }}_{\rm{0}}}{\rm{ + }}{{\rm{\mu }}_{\rm{2}}}} \right){{\rm{I}}_{{\rm{F2}}}}}\\ {\dfrac{{{\rm{dR}}}}{{{\rm{dt}}}}{\rm{ = }}{{\rm{\gamma }}_{\rm{1}}}{{\rm{I}}_{{\rm{F1}}}}{\rm{ + }}{{\rm{\gamma }}_{\rm{2}}}{{\rm{I}}_{{\rm{F2}}}}{\rm{ - \omega R - }}{{\rm{\mu }}_{\rm{0}}}{\rm{R}}} \end{array}} \right.}$$ The model involves 7 classes and 14 parameters. Each equation represents the change rate of the number of people in each class in unit time, and the right side includes the moving in and out of items that lead to the change of class population. The unit time of this model is one year.
Λ is the constant recruitment in the system. β1 and β2 are the transmission rates of infectious drug-sensitive TB cases and rifampin resistant TB cases (RR-TB). κ is the progressive rate from the exposed to the infectious; ρ is the progressive rate from drug-sensitive TB to RR-TB; σ is the detection rate of the infectious; γ1 and γ2 are the successful treatment rates of detected patients with infectious drug-sensitive TB and RR-TB, respectively; ω is the disease recurrence rate from the recovered population; τ1 and τ2 are the drug resistance rates of new patients and recurrent patients, respectively; and μ0 is the natural mortality rate, while μ1 and μ2 are the fatality rates of TB in infectious drug-sensitive TB cases and RR-TB cases, respectively. The transmission diagram is shown in Figure 1.
We collected the reported incidence of pulmonary TB in Shanghai from 2004 to 2017 provided by the Public Health Science Data Center, of which 2004−2012 were used as training data and 2013−2017 years were used as test data. The values of the parameters were determined by the reports of earlier studies and adjusted according to TB data, then the incidence of pulmonary TB in Shanghai was estimated for the near future. The incidence of pulmonary TB was numerically defined as the number of new reported cases of pulmonary TB within each year as a proportion of the number of average annual population.
The parameters in the model were adjusted to simulate the effect of three different TB prevention and control strategies. We reduced the values of parameters β1, β2, and ω to simulate reducing the probability of infection or reinfection of susceptible and recovered patients (assuming 60% of recurrent patients are due to reinfection) to simulate strengthening personal protection and isolation of active cases during contagious period. The effect of preventive treatment on LTBI cases was evaluated by reducing the rate of progression (κ) of the exposed group to the infectious groups. We reduced the recurrence rate (ω) of the recovered group to study the impact of recurrence rate on the TB epidemic.
We set the initial values of the model classes as S (0) = 14,453,131, E (0) = 3,834,319, IU1 (0) = 6,462, IU2 (0) = 333, IF1 (0) = 7,011, IF2 (0) = 361, R (0) = 48,194, and the values of parameters are shown in Table 1. The first curve of each panel in Figure 2 shows our prediction of the incidence of pulmonary TB in Shanghai under current strategies. We predicted that the estimated incidence of pulmonary TB in Shanghai will continue to decline from 2004 to 2050. In 2025, the incidence of TB in Shanghai was estimated to be 24.27/100,000, which will achieve the WHO’s goal in 2025 (<55/100,000). However, the incidence was estimated to be 20.81/100,000 in 2035, still far from the goal set for 2035 (<10/100,000).
Figure 2 shows the impact of 3 different prevention and control strategies on pulmonary TB in Shanghai. The incidence will decrease slightly with the values of parameters β1, β2 and ω reduced (Figure 2A). The incidence of pulmonary TB in Shanghai in 2035 will be 19.69/100,000 when the parameters dropped by 50%. Reducing the progressing rate (κ) of the exposed group to the infectious groups, the incidence of pulmonary TB in Shanghai will decrease significantly (Figure 2B). In 2035, the incidence will be 11.55/100,000 with the parameters κ dropped by 50%. The incidence of pulmonary TB in Shanghai will be slightly decreased by reducing their recurrence rate (ω) (Figure 2C). With the recurrence rate reduced by 50%, the incidence of pulmonary TB in Shanghai will be 19.08/100,000 in 2035.
HTML
-
In this study, a dynamic transmission model concerning both RR-TB and a relapse of TB was established, and the RR-TB rate of recurrent patients was distinguished from that of new patients. Current prevention and control strategy for TB in Shanghai was estimated to be able to achieve the goal set forth by the WHO in the End TB Strategy in 2025 but were not sufficient to achieve the goal in 2035. The target was estimated to be unachievable due to many reasons including the large number of latent infections (7), coinfections with HIV / AIDS (8), and a large migrant population (9).
Among the three prevention and control strategies, strengthening preventive treatment for LTBI cases had the best effect on TB epidemic control. The incidence of pulmonary TB in Shanghai was estimated to decrease to 11.55/100,000 when the progressing rate dropped by 50%, which was close to the goal for 2035. The other two strategies were estimated to only reduce the incidence of pulmonary TB slightly. This indicated that the large number of LTBI cases was the reason why the incidence of TB was not decreasing as fast as expected. The WHO estimated that the global LTBI population was close to 2 billion, accounting for 1/3 of the global population (4).
Carrying out preventive treatment for latent infections is based on strengthening screening for latent infections. China has previously shown the ability to conduct large-scale screenings for an infectious disease in a large city (10), which indicates that it is possible to strengthen screening. Considering the large scope of consumption in the process of the project, screening for latent TB infections using tuberculin skin testing and/or interferon gamma release assays can be carried out regularly in high-risk groups and areas.
This study was subject to some limitations. For example, the parameters used in model operation and prediction were fixed values, but the parameters in the model change dynamically with time in real life. The fixed parameter value could only predict long-term trends for TB but not short-term fluctuations. In addition, considering the difficulty of obtaining the parameters, the model only set 7 classes without further subdivisions, so there was still a gap with real circumstances of TB in Shanghai. Further studies could consider dividing the population of recovered individuals into subgroups with different recurrence rates according to their recurrence risk.
-
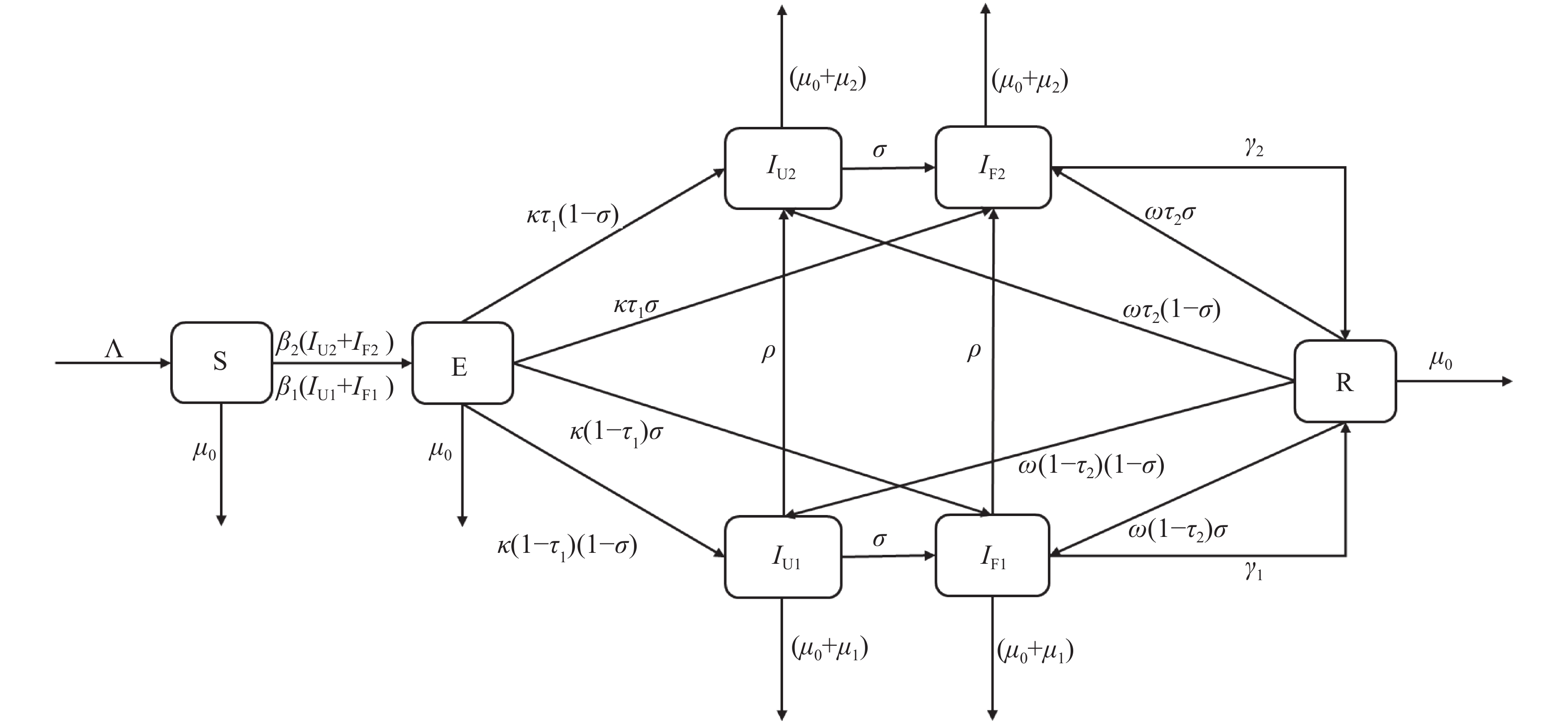 Figure 1.
Figure 1.The flow diagram of tuberculosis model considering rifampicin resistance and recurrence.
S referred to people who are not infected with Mycobacterium tuberculosis (M. tb); E referred to people infected with M. tb but were not yet infectious; I referred to patients with infectious pulmonary tuberculosis (TB); IU1 referred to the undetected and drug sensitive population; IU2 referred to the undetected and rifampicin resistant population; IF1 referred to the detected and drug sensitive population; IF2 refers to the detected and rifampicin resistant population; and R referred to TB patients who have been successfully treated. β1 and β2 are the transmission rates of infectious drug-sensitive TB cases and rifampin resistant TB (RR-TB) cases. κ is the progressive rate from the exposed to the infectious; ρ is the progressive rate from drug-sensitive TB to RR-TB; σ is the detection rate of the infectious; γ1 and γ2 are the successful treatment rates of detected patients with infectious drug-sensitive TB and RR-TB, respectively; ω is the disease recurrence rate from the recovered population; τ1 and τ2 are the drug resistance rates of new patients and recurrent patients, respectively; and μ0 is the natural mortality rate, while μ1 and μ2 are the fatality rates of TB in infectious drug-sensitive TB cases and RR-TB cases, respectively.Parameter Definition Estimated value Λ Constant recruitment of the population 486,245 β1 Transmission rate of infectious drug-sensitive TB cases 8.69×10−12 β2 Transmission rate of infectious RR-TB cases 2.52×10−10 k Progressive rate from the exposed to the infectious 1.65×10−3 τ1 Drug resistance rate of new patients 2.39×10−2 σ Detection rate of the infectious 6.20×10−1 ρ Progressive rate from drug-sensitive TB to RR-TB 8.85×10−2 γ1 Treatment successful rates of infectious drug-sensitive cases 9.14×10−1 γ2 Treatment successful rates of infectious RR-TB cases 8.99×10−1 ω Recurrence rate from recovered 5.94×10−3 τ2 Drug resistance rate of recurrent patients 1.25×10−1 μ0 Natural mortality rate 7.46×10−3 μ1 Fatality rates of TB in infectious drug-sensitive TB cases 9.32×10−3 μ2 Fatality rates of TB in infectious RR-TB cases 2.26×10−2 Abbreviations: TB=tuberculosis; RR-TB=rifampin resistant TB. Table 1. Definitions and estimated values of parameters.
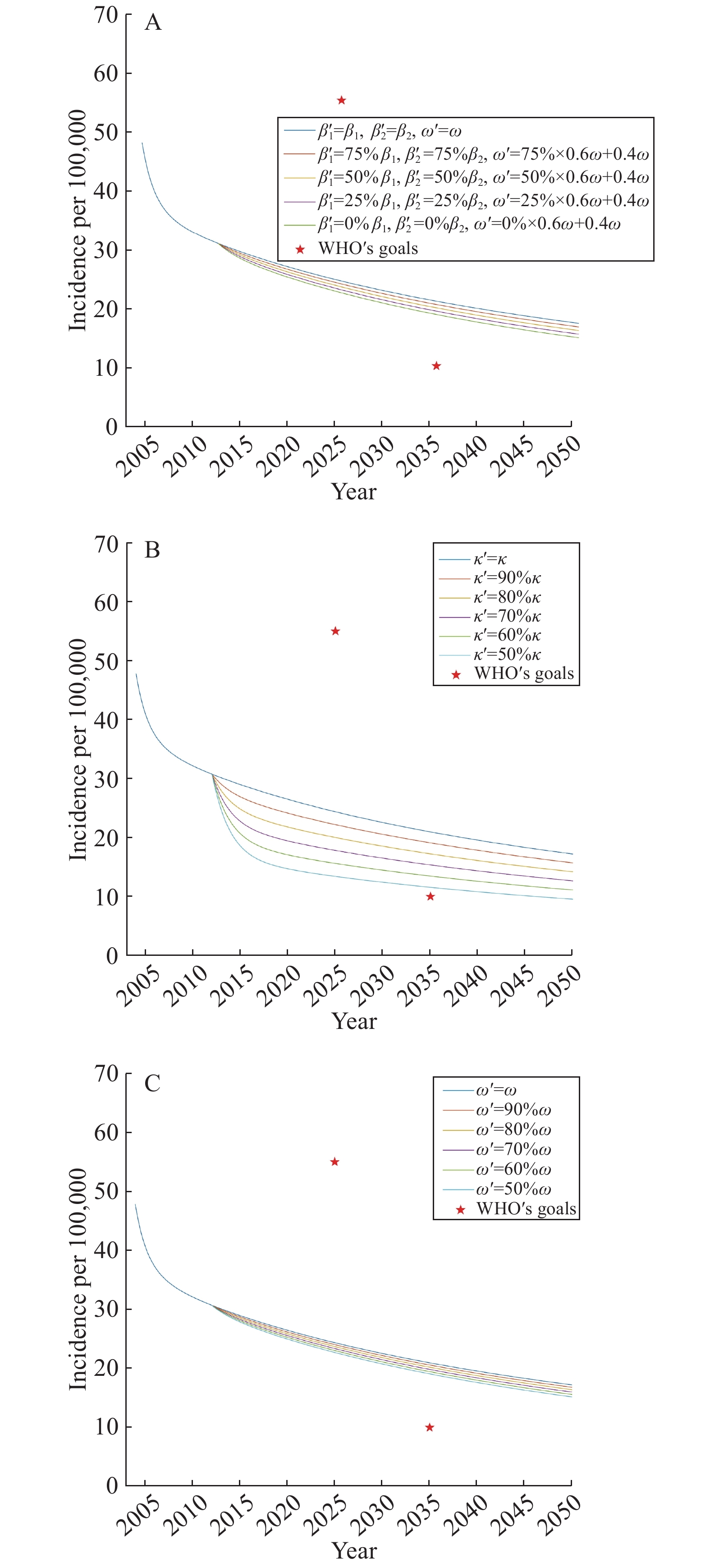 Figure 2.
Figure 2.Predictions of the incidence of pulmonary TB in Shanghai with different parameters. (A) Reducing the values of parameters β1, β2 and ω. (B) Reducing the values of parameter κ. (C) Reducing the values of parameter ω.
Funding: Key Joint Project for Data Center of the National Natural Science Foundation of China and Guangdong Provincial Government (U1611264); and the National Natural Science Foundation of China (91546203, 91846302).
| Citation: |



 Download:
Download:





