-
On October 6, 2020, Jidong County CDC received a report that a family in Sihai Community, Xingnong Town had a suspected foodborne poisoning incident. By the investigation of the county, municipal, and provincial CDC, the incident was due to consumption of the local homemade specialty food, a sour soup, for breakfast on October 5. In the homemade processing and storage, this food was contaminated by Burkholderia gladioli pathovar cocovenenans (B. cocovenenans) which can produce bongkrekic acid (BA), resulting in deaths for all persons exposed due to poisoning. The case attack and fatality rates were both 100% in the persons who consumed the sour soup. Improper processing and storage of fermented corn flour products can cause BA poisoning.
-
On October 4, a total of 12 persons involving 5 families gathered for lunch and dinner. At around 8∶00 am on October 5, the 12 persons had breakfast together and left separately. Among them, 9 persons consumed the sour soup , while 3 did not and all the 12 persons had consumed the other food items. The 9 persons then successively developed gastrointestinal symptoms such as nausea, vomiting, and abdominal pain. Finally, all 9 cases died after treatment.
On October 6, the investigation revealed that the 9 cases included 4 males and 5 females with an average age of 61 years (range: 45–72 years). Detailed clinical data were collected on the initial patient and her husband. Physical examination of the initial case showed tenderness in the upper abdomen. Laboratory abnormalities include progressive dysfunction of liver function, renal function, and coagulation function in her and her husband, and imaging indicated diffuse changes in the liver (Table 1). The attack rate was 100% in the persons who consumed sour soup and the attack rate was 0% in those who did not consume it, which suggested that the sour soup was the likely source of exposure. The median latency period was estimated as 3 hours (range: 2–8 hours) according to the time of consumption of sour soup and the onset time of the case. The median course of disease in 9 cases was 53 hours (range: 20–341 hours). The patients and cases were numbered 1–9 according to the latency period from short to long (Figure 1). Patient 9 had the longest latency period, and he returned home after receiving prescription medication from the outpatient department. He then died at home with the shortest course of illness, which was only 20 hours.
Patient Gender Age
(years)Latency period (h) Course of disease (h) Clinical manifestation Physical examination Liver function Coagulation function Renal function Imaging Nausea, vomiting Diarrhea Dizziness, fatigue Oliguria Tenderness in the upper abdomen ALT (U/L) AST (U/L) PT
(s)APTT
(s)PLT
(109/L)UREA
(mmol/L)CREA
(μmol/L)Abdominal CT scan Initial patient’s husband Male 49 4 61 + + + + + 22,640↑ 43,900↑ >120↑ 88.3↑ 30↓ 8.87↑ 466↑ Liver diffuse lesions Initial patient Female 47 2 341 + − + + − 7,199↑ 10,630↑ 71.4↑ 46.6↑ 27↓ 1.84↓ 213↑ Liver diffuse lesions Note: Marks: + : indicates symptoms that do occur; -: indicates symptoms that do not occur; ↑: means increasing; ↓: means decreasing.
Abbreviations and reference ranges: ALT: Alanine aminotransferase 0–40 U/L; AST: Aspartate aminotransferase 0–40 U/L; PLT: Platelets (100–300)*109/L; APTT: Activated partial thromboplastin time 23–35 s; PT: Prothrombin time 10.5–13 s; UREA: Urea nitrogen 2.3–7.2 mmol/L; CREA: Creatinine 44–110 mmol/LTable 1. The clinical characteristics list of two typical cases in the foodborne bongkrekic acid poisoning incident in Jidong County, Heilongjiang Province, 2020.
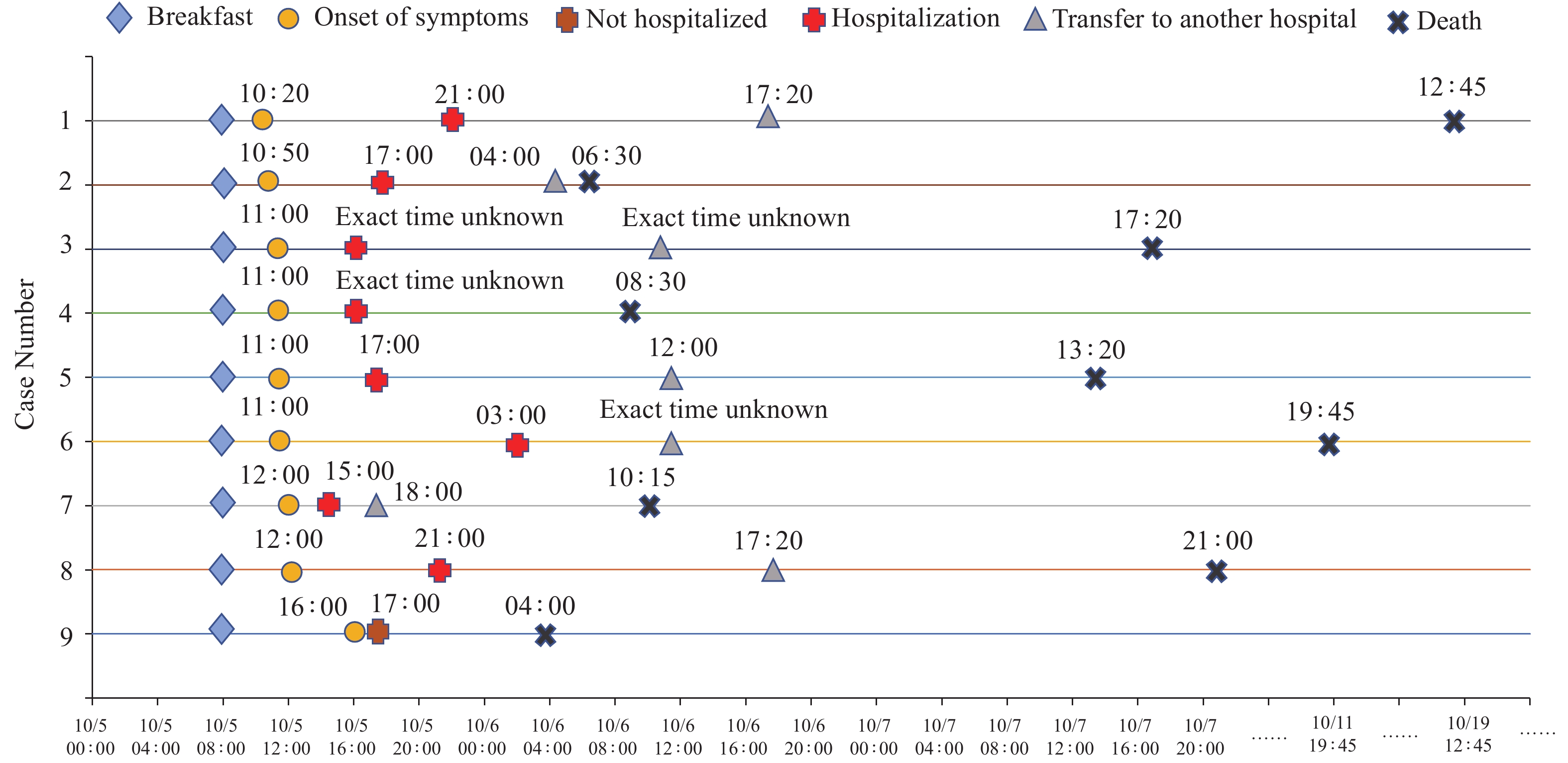 Figure 1.
Figure 1.Sequence diagram of the course of disease of patients in the foodborne bongkrekic acid poisoning incident in Jidong County, Heilongjiang Province, 2020.
According to the investigation, the process of making the homemade sour soup was as follows: one year ago, the corn was soaked in water for about a month to ferment. After mill grinding, the corn husks were filtered out in the water, and the delicate parts were kept to be dried in flour bags and formed into dough and then noodles with a specialized tool. It was consumed as soon as the noodle-based sour soup was ready and the rest of the dough was put in the refrigerator and frozen. This fall, because the refrigerator was used to store other foods, the dough was made into cornmeal powder and then stored in the refrigerator again to save space. After the corn dough was taken out, it was first exposed to air outside and covered with a simple porous plastic net. After drying for a day, it was transferred to dry in the house due to cloudy and rainy weather.
On October 5, the local public security department extracted all the types of residual food and detected them. No poisonous substances such as cyanide, organophosphorus, carbofuran, psychostimulant, or tetramine were found. On October 7, the municipal CDC tested all the types of food and a patient’s gastrointestinal decompression fluid for salmonella, and the results were negative. The local hospital tested the food and found the aflatoxin was in excess. As this toxin is a common contaminant of corn, and it generally does not cause acute poisoning manifestations as the latency period is usually 2–3 weeks (1), which caused it to be excluded. On October 10, the provincial CDC detected BA in the remaining raw material for the sour soup, the corn flour, and the gastrointestinal decompression fluid. In accordance with national standard (2), the concentration of BA was 330 mg/kg and 3 mg/L, respectively. Combined with the epidemiological investigation result, the patient’s clinical manifestations and laboratory test results, the investigation team confirmed this poisoning incident was caused by BA when bacteria contaminated the corn flour and was used to make the sour soup.
-
Local CDC and the National Early Warning Information Dissemination Center has issued a warning message about BA poisoning. China CDC tracks the handling of incidents, provides technical guidance on epidemiological investigation and sampling detection, and at the same time obtains information from surveillance systems and carries out risk assessments regularly.
-
Based on the consumption of staple food of 100 g per person, the BA concentration of corn flour and the remaining raw food material collected on the scene, was 22–33 times higher than the lethal dose of 1–1.5 mg (3) and resulted in all 9 deaths. Laboratory studies have shown that coconut, corn, and other foods that are rich in oleic acid, are suitable for the growth of B. cocovenenans at a neutral pH of 22–30 ℃. When B. cocovenenans is cultured on coconut medium under ideal conditions, toxin production can reach 2–4 mg/g by the second day of culture (4). Although it is not clear how the corn flour used to make the sour soup was contaminated in this incident, we can learn from the production process that the poisoned sour soup was made in the same batch as last year. There was no abnormal consumption last year, and the contamination probably occurred after the food was taken out of the refrigerator. The corn dough was likely contaminated with bacteria when it was dried outside. The natural air drying speed was slow as the environment likely had poor ventilation, high relative humidity, and a suitable temperature for bacterial growth. These factors provide favorable conditions for the bacteria to multiply and produce the toxin. Despite the destruction of B. cocovenenans during cooking, the BA produced by them has a heat-stable character. Therefore, the storage, processing, and sanitary conditions of raw food materials were closely related to the occurrence of poisoning.
In Indonesia and Mozambique, the reported case fatality rate of BA poisoning were 60% and 32%, respectively (4-6). As of January 1, 2004, China CDC launched the Public Health Emergency Management Information System, which is a surveillance system for public health emergencies that may occur or have already occurred, which is reported online by medical and health institutions at all levels. The surveillance data showed that 15 BA poisoning incidents, 136 poisoned individuals, 36 resulting deaths, and a case fatality rate of 26.47% was reported during 2010–2019 in the mainland of China. These occurred in the provincial-level administrative divisions of Yunnan, Guizhou, Guangxi, Guangdong, Liaoning, and Shandong. Compared with 545 such incidents from 1953–1994, 3,352 persons were poisoned, among which 1,401 died (case fatality rate was 41.80%), and the scale showed a significant decline (7). According to the reported 15 incidents of foodborne poisoning caused by BA, there was 1 incident of sour soup poisoning at Liaoning Province in northeastern China, in which 4 persons were poisoned and all died. There were 2 incidents of poisoning caused by nonfermented rice noodle product at Guangdong Province in southern China, 8 people were poisoned and 5 died (case fatality rate was 62.5%). There were 5 incidents of poisoning caused by Diaojiangba (hanging syrup cake) in Yunnan Province, 47 people were poisoned and 15 people died (case fatality rate was 32%), suggesting that different types of starch products may lead to different case fatality rates.
There are few BA detection reports for past incidents, and they are mainly inferred based on exposure and clinical manifestations. The reason why the fatality rate of this incident was much higher than that of previous incidents was likely related to the exposure dose being much higher than the lethal dose.
The Health Emergency Information Platform for Poisoning Emergencies (an information system for emergency work for poisonings in provincial-level medical and health institutions) showed that up to July 2020 among the 81 institutions that were provincial CDCs, provincial treatment bases for poisoning, and designated medical institutions in China, only 7% had reserved and had access to the detection technology of BA in their daily work. It took 5 days and 6 days to get the qualitative and quantitative test results in this incident, respectively, which represents a shortcoming in the detection capacity of early and rapid diagnosis of BA.
At the same time, studies on the toxicokinetics of BA are lacking. There is no specific antidote (8) or standardized treatment guidelines for BA poisoning. The treatment of patients is mainly to terminate toxic contact, remove toxins that have not been absorbed in the body, and provide symptomatic support treatment. If the cases of this incident were treated in time at a hospital capable of treating severe poisoning, the case fatality rate may be reduced.
The investigation had several limitations. Because the patient who made the poisoned food fell ill and died, it was impossible to know all the details of how it was prepared. Most patients had a short course of illness with limited or unavailable clinical records. Not all patients had biological specimens collected for BA quantitative detection.
In high-risk areas, prevention of exposure to B. cocovenenans and BA and safer fermentation processes should be adopted. Meanwhile, training in BA poisoning and confirmative testing in primary health care facilities should be strengthened to improve emergency response capacity for timely diagnosis and response. In addition, scientific institutions should conduct studies on the distribution of B. cocovenenans, the laws of toxin production, and toxicokinetics of BA and develop commercial products for rapid detection of toxins in food.
HTML
| Citation: |



 Download:
Download:




