-
Congenital hearing loss affects approximately two infants per 1,000 live births in the United States (USA), making it one of the nation’s most common developmental disabilities (1). When left undetected, permanent congenital hearing loss can negatively impact children through delays in their speech, language, social, and emotional development (2). Children who are identified as deaf or hard of hearing (D/HH) should begin receiving intervention services as early as possible to help mitigate the potential adverse effects (3).
Although the importance of identifying hearing loss during the first few months of life was recognized almost 80 years ago (4), nationwide efforts to reduce late identification of congenital hearing loss did not begin until the 1990s. This was a result of advances in newborn hearing screening technologies, increased epidemiologic evidence that many D/HH children were not identified early (5), and resources from the federal government (6). By 2000, all USA states had started implementing programs to support universal newborn hearing screening (UNHS) in hospitals, early diagnosis, and enrollment in intervention for children diagnosed as D/HH. These state programs are commonly referred to as the Early Hearing Detection and Intervention (EHDI) programs (7).
In this paper, we outline the initial implementation of EHDI in the USA, followed by a review of the key factors that influenced the evolution of EHDI programs over the past 20 years. We discuss national and state efforts in establishing and promoting UNHS-related legislation, best practices, and developing public health infrastructure to help ensure the provision of hearing screening, diagnostic, and intervention services. We also highlight challenges that EHDI programs have experienced and discuss potential directions for continued improvements in the future.
-
State and federal laws have served as an important component in many public health achievements (8) including EHDI. Analyses have shown that states that implemented UNHS related legislation had significantly higher newborn hearing screening rates than states with no legislation (9). In the early 1990s, Hawaii and Rhode Island became the first states to pass UNHS related legislation. While the legislative requirements varied, by 2003, 37 of the 50 states in the USA had enacted some type of UNHS legislation. In 2016, only 4 states (Idaho, North Dakota, South Dakota, Washington) did not have laws related to hospital newborn hearing screening (10).
Legislative support of UNHS/EHDI by the federal government began with the Children’s Health Act of 2000 (11). This Act authorized two federal agencies — the Health Resources and Services Administration (HRSA) and Centers for Disease Control and Prevention (CDC) — to support EHDI activities at the state level. The 2017 EHDI Act (S. 652, PL 115-71) authorizes HRSA to continue awarding funds to states, territories, and healthcare providers for continuous improvement of EHDI programs. These projects help to identify effective strategies to address screening, loss to follow-up, diagnosis and services, enrollment into early intervention services, family engagement and support systems, and professional education. The Act authorizes CDC to provide both funding and technical assistance to support the development and implementation of data management and tracking systems within state EHDI/UNHS programs and to develop national data standards and track progress towards achievement of EHDI goals.
-
Awareness of infant hearing loss and the need for early identification has been endorsed by a number of professional organizations, including the Joint Committee on Infant Hearing (JCIH) beginning with their 1994 position statement. JCIH is comprised of representatives of member organizations from the fields of audiology, otolaryngology, pediatrics, and nursing and was established in 1969. Its primary activities have been the “publication of position statements summarizing the state of the science and art in infant hearing and recommending the preferred practice in early identification and appropriate intervention of newborns and infants at risk for or with hearing loss” (12).
Building on the 1994 statement, the JCIH 2000 position statement (13) identified Principles and Guidelines for state EHDI programs, which continue to be relevant twenty years later. The 2000 position statement highlighted public health tracking and surveillance systems as essential for the early detection and intervention of congenital hearing loss and established benchmarks to monitor compliance and outcomes at each step in the EHDI process. These benchmarks, often referred to as the EHDI 1-3-6 plan, call for hearing screening no later than 1 month of age, diagnosis no later than 3 months of age for infants not passing the screening, and enrollment into intervention no later than 6 months of age for those identified as D/HH.
Over the past 20 years there has been a growing body of evidence linking UNHS, early identification of hearing loss, and timely entry into intervention with improved language outcomes, lasting benefits for the child’s development, and cost savings (14-18). Based on these findings and expert consensus opinion, JCIH updated its best practice guidelines in 2007 and 2019. The JCIH 2007 position statement reaffirmed the 1-3-6 plan and emphasized the importance of implementing state-based information infrastructure to monitor the quality of EHDI services (19). In its latest position statement (3), JCIH recommended that states who already meet the 1-3-6 benchmarks strive to meet a 1-2-3 month timeline (screening completed by 1 month, audiology diagnosis by 2 months, enrollment in early intervention by 3 months). It also recommended enhanced information infrastructure that interfaces with clinical electronic health records and population-based information systems, to support improved performance and quality measurement and reporting.
-
With enactment of the Children’s Health Act of 2000, federal funding became available through the CDC and HRSA for EHDI activities. The funding and assistance provided by CDC to state programs supported the development and implementation of data management and tracking systems, called EHDI Information System (EHDI-IS). These confidential, computerized, population-based systems serve as tools for states to collect and consolidate data at different stages of the EHDI process to support effective tracking and follow-up of hearing services for all infants. Over the past 20 years, these systems have evolved from basic data repositories with limited case management and reporting capabilities to complete, integrated information systems. Today most EHDI-IS provide near real-time and direct data access, as well as decision support for public health officials to track and monitor care and service provision for infants and children at risk of congenital hearing loss. (Figure 1).
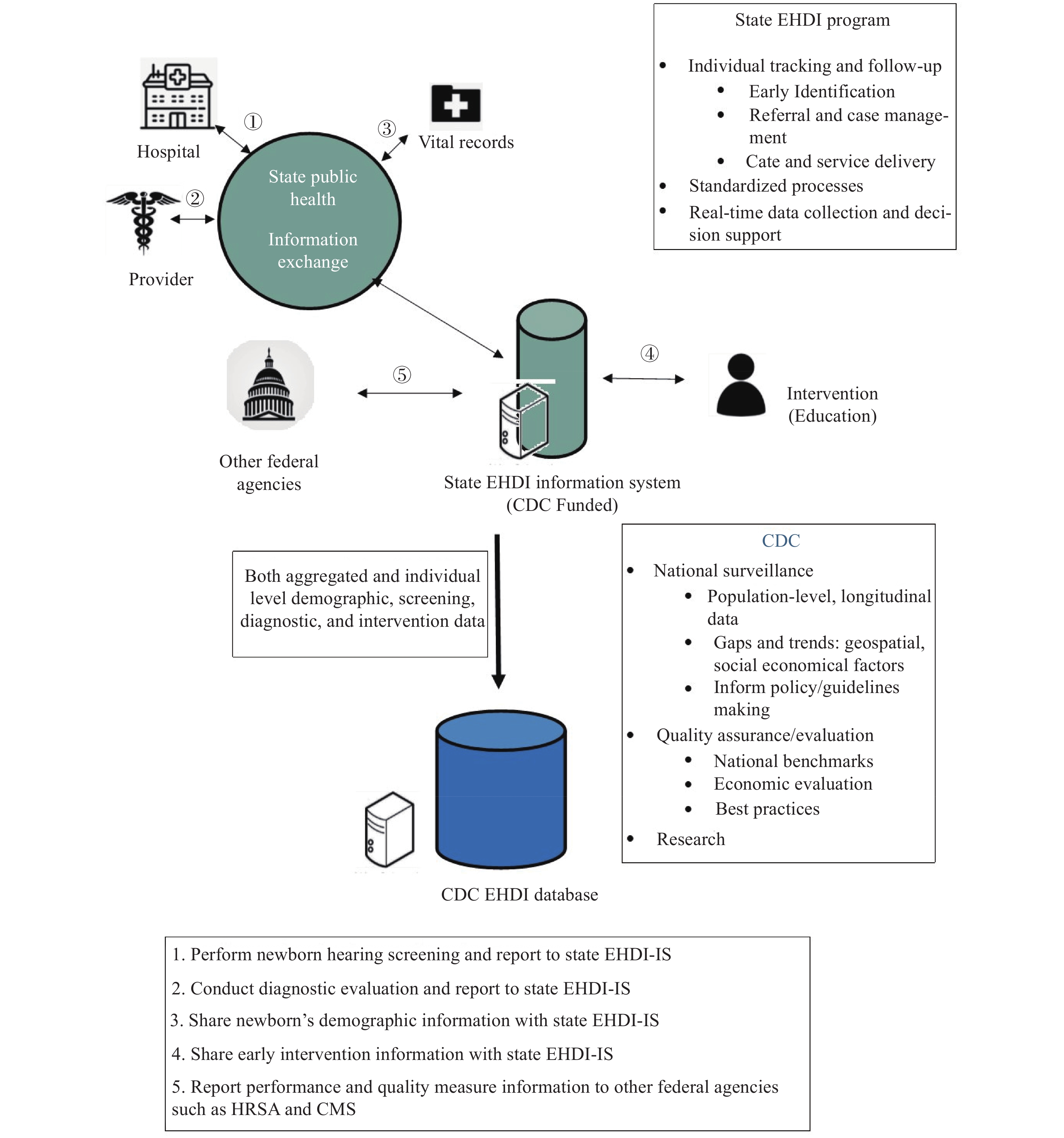 Figure 1.
Figure 1.Federal and state Early Hearing Detection and Intervention (EHDI) tracking and surveillance information infrastructure. Abbreviation: CDC=Centers for Disease Control and Prevention; EHDI-IS=EHDI Information System; HRSA=Health Resources and Services Administration; CMS=Centers for Medicare and Medicaid Services.
Since 2007, states annually submit data from their EHDI-IS to CDC through the Hearing Screening and Follow-up Survey (HSFS) (20), which is used to assess the nation’s progress towards the EHDI 1-3-6 benchmarks. Over the years there has been a steady increase in the documented percentages of infants meeting these benchmarks (Figure 2). The percentage of infants screened by one month of age increased from an average of 91.6% during 2005–2006 to 95.5% during 2016–2017. During the same timeframe, the infants meeting the intervention benchmarks increased by more than ten percentage points (from 32.2% to 44.3%). The biggest improvement was in diagnosis. During 2005–2006, only approximately 15.0% of infants who did not pass their hearing screening were diagnosed before three months of age. The percentage of infants meeting this diagnosis benchmark increased to 40.0% during 2010–2011, and then to nearly 50.0% during 2016–2017.
-
Although timely completion of hearing screening has been consistently achieved for most newborns in the past decade, challenges remain in ensuring the timely receipt of follow-up diagnostic and intervention services for all children at risk. During 2016–2017, among all reported cases nationwide, less than 50% of infants not passing hearing screening were confirmed to have received diagnosis before the recommended benchmark of 3 months of age, and less than half of children identified as D/HH were enrolled in intervention before 6 months of age. Wide variations in meeting these benchmarks exist at the state level, with some programs performing well above the national average, and others having not been as successful. First, such variations could be attributed to lack of effective follow-up strategies; reductions in resources available to some programs, and differences in state statutes, regulations, or policies. Second, differences in the infrastructure and capabilities of the state-based EHDI-IS limit the ability of some programs to accurately identify, match, collect, report, and analyze data on all births. Some states still largely rely on old technologies, such as mail and fax to collect and report EHDI data. Variation in data definitions among state programs can also contribute to differences in the reported results, making it difficult for CDC to monitor performance (21-22). Closely related to the implementation of modern information systems is the implementation of systematic evaluation and quality assurance programs. Some state EHDI programs have not had time or resources yet to implement such systematic evaluation and quality assurance programs. Finally, geographic, racial, and socio-economic disparities in the provision of diagnostic and intervention services persist within many states (23-25). Given the clinical resources that are needed to adequately diagnose congenital hearing loss early, and the economic resources associated with it, it is not surprising that people living in rural, remote areas and/or with lower socio-economic status may be more likely to experience delays in receiving recommended services.
-
Over 95% of babies in the USA now receive a hearing screening before one month of age, up from only 20% in 1999. Each year in the USA, over 6,000 infants who are D/HH are being identified early. With this progress, more children, along with their families, have the opportunity to experience improved outcomes in language development and overall well-being (1,26).
Sustaining these achievements and advancements in EHDI programs will likely require concerted efforts from all stakeholders, including government agencies, research institutions, hospitals, audiologists and pediatricians, rehabilitation and intervention service providers, and others.
First, it is important for public health agencies to continue highlighting the value of identifying children who are D/HH as early as possible among healthcare providers and administrators and, contingent on their funding appropriations, to assist (e.g., technical and financial) with implementation of best practices. This includes ongoing training at the community level, which can help ensure families with children at risk to be full participants in the EHDI process. Second, it is important to enhance population-based public health surveillance systems that can provide timely and accurate data on all newborns. To enhance tracking, follow-up, case management, and reporting, such systems may wish to adopt nationally recognized functional standards, data definitions, and quality measures. They may also leverage evolving health information technologies for information exchange and analysis. In addition, increased efforts might be considered to improve the availability of specialized services to under-served populations (e.g., using telemedicine). With all stakeholders continuing to collaborate and coordinate their efforts, infants and young children with permanent hearing loss will be more likely to acquire the “fundamental language, social, and cognitive skills that provide the foundation for later schooling and success in society” as foreseen 30 years ago in Healthy People 2000 (27).
Disclaimer: The opinions expressed in this article are the authors’ own and do not reflect the view of the Centers for Disease Control and Prevention, the Department of Health and Human Services, or the United States government.
HTML
State and Federal Laws in the USA
Best Practices
Public Health Surveillance
| Citation: |




 Download:
Download:





