-
In 2004, the mortality rate among children under five in China was 25 per 1,000 live births, with approximately 20% of the deaths attributable to birth asphyxia (4). Before 2004, neonatal resuscitation training had been conducted in few areas of China. Some medical universities, medical associations, and international non-governmental organizations developed small-scale training courses in a few provincial-level administrative divisions (PLADs) and donated neonatal resuscitation equipment to impoverished areas to promote neonatal resuscitation (5). However, due to the limited coverage and sustainability of professional training, neonatal resuscitation was not given adequate attention (6). In July 2004, the Maternal and Child Health (MCH) Department of the then Ministry of Health launched the Newborn Resuscitation Programme (NRP) nationwide to explore a multi-sectoral cooperation mechanism for the promotion of neonatal resuscitation techniques. Over the past 15 years of implementation, neonatal resuscitation training in facilities providing midwifery has expanded. The first NRP stage was launched in 20 PLADs in western and central China between 2004 and 2009, and was subsequently expanded to all 31 PLADs and Xinjiang Production and Construction Corps (XPCC) of the mainland of China during the second and third phases during 2011–2016 and 2017–2021. The objective of the NRP was to ensure that at least one trained attendant proficient in neonatal resuscitation skills was present at every delivery, with the ultimate goal of reducing the incidence of neonatal asphyxia and the neonatal mortality rate (1). The programme also established a collaborative resuscitation system in hospitals with quality improvement training and supervision and project management (7).
-
With official government management, technical guidance of academic associations and specialized institutions, and financial support from social organizations, multiple parties worked together to expand NRP’s coverage and ensure smooth implementation of related activities (7). The mechanism was characterized by well-defined departmental responsibilities, rational division of labor, and strong coordination and communication. National and provincial health administrative departments managed project implementation and provided policy support. Academic associations and specialized facilities organized expert teams for technical support based on domestic and foreign academic exchange platforms. Social organizations provided financial support and conducted publicity and promotional activities through various channels to raise public awareness and understanding of neonatal resuscitation.
-
Based on a “Training of Trainers” approach, cascaded training was implemented in teams composed of international, national, provincial, and county instructors. China formulated its guidelines for neonatal resuscitation by introducing the training mechanism from the American Academy of Pediatrics NRP curriculum and adapting the technical processes of resuscitation based on local healthcare settings. Using the guidelines, international experts introduced neonatal resuscitation techniques in China and trained and assessed a national training team of 33 experts. Each instructor was assigned 8 trainees and used theoretical education combined with simulated demonstrations supported by related teaching equipment (8). From 2004 to 2018, the national experts trained experts from the 31 PLADs and XPCC of the mainland of China and established provincial-level training teams composed of more than 900 facilitators. Prefecture- and county-level training teams were established in a similar cascading approach. The programme developed an online training and assessment platform with the quality of technical training enhanced through regular supervision, refresher trainings, and quality control exercises. Activities like the neonatal resuscitation skills competition were used to promote technical training and its application (8).
-
To enhance collaboration among obstetrics, neonatology, anesthesiology, and other specialties, and strengthen hospital-based professional training in neonatal resuscitation techniques, in 2009, China formulated a plan to establish a Neonatal Resuscitation Leadership Group in Health Facilities, which was subsequently replicated in all county-level health facilities. In 2014, the then General Office of the National Health and Family Planning Commission issued the Management System for Newborn Safety in Health Facilities (Trial), requiring primary, secondary, and tertiary general hospitals and secondary and tertiary MCH institutions to ensure that “at least one health staff member equipped with neonatal resuscitation techniques was present at every delivery.” Delivery rooms had to have equipment and medicines for neonatal resuscitation and rescue. The management system listed coverage of resuscitation techniques as a performance indicator for health facilities, laying a policy foundation for neonatal resuscitation technical training in various regions, thus successfully promoting neonatal resuscitation techniques. The National Health Commission emphasized the need to strengthen neonatal resuscitation technical assessment and provided relevant support with multiple documents, including the Maternal and Child Safety Action Plan, Guidelines for the Construction and Management of the Treatment Centers for Critically Ill Pregnant Women and Newborns, MCH facility review and performance appraisals, and establishment of neonatal care departments in MCH hospitals (7). These efforts provided an impetus to translate empirical experience into policy, making neonatal resuscitation training a policy requirement for health facilities.
-
From 2008 to 2009, the National Center for Women and Children’s Health, Chinese Center for Disease Control and Prevention, surveyed 322 hospitals to evaluate the effectiveness of NRP implementation in the first stage (2004–2009) (1). Efficacy of NRP implementation in the second stage (2011–2016) was evaluated by mail survey of 347 hospitals from October to November 2016 (9). Detailed descriptions of sampling methods and results have been published (1,9). The 2016 NRP evaluation showed that more than 90% of health facilities in programme areas established an in-hospital neonatal resuscitation working group responsible for technical training and quality control. Neonatal resuscitation training was conducted in more than 95% of enrolled health facilities (9). During NRP implementation, the incidence of neonatal asphyxia (defined as Apgar score ≤7 at 1 minute) decreased by 77.5%, from 6.32% in 2003 to 1.42% in 2020, while neonatal mortality due to birth asphyxia in the delivery room decreased by 75%, from 0.76‰ in 2003 to 0.19‰ in 2020 (Table 1, Figure 1). As a result, neonatal resuscitation techniques have been substantiated to be lifesaving for newborns.
Year Live births Asphyxia incidence Asphyxia death Cases Crude rate (%) Z* P Cases Crude rate (‰) Z* P The first stage of NRP† 2003 237,140 14,998 6.32 ‒77.671 <0.001 179 0.76 ‒7.782 <0.001 2004 295,567 16,395 5.55 169 0.57 2005 317,069 14,254 5.50 166 0.52 2006 344,147 15,304 4.45 157 0.46 2007 408,247 13,933 3.41 168 0.41 2008 428,261 12,594 2.94 146 0.34 The second stage of NRP§ 2010 335,190 7,810 2.33 ‒20.162 <0.001 81 0.24 ‒2.686 0.007 2011 385,694 8,755 2.27 86 0.22 2012 407,451 8,719 2.14 85 0.21 2013 434,287 8,555 1.97 83 0.19 2014 515,481 9,227 1.79 85 0.16 Surveillance data from MCH institutions¶ 2017 2,694,010 43,032 1.60 ‒18.794 <0.001 1,273 0.47 ‒21.888 <0.001 2018 2,488,254 36,733 1.48 1,250 0.50 2019 2,602,198 35,961 1.38 560 0.22 2020 2,400,961 34,155 1.42 446 0.19 Abbreviation: MCH=maternal and child health; NRP=neonatal resuscitation programme; PLADs=provincial-level administrative divisions.
* Cochran-Armitage trend test. A negative value of Z implies a decreasing trend of asphyxia incidence and mortality rate. P value <0.05 is considered statistically significant.
† The first stage of NRP was launched in 20 PLADs of western and central China between 2004 and 2009, and the final effectiveness evaluation was conducted.
§ The second stage of NRP was launched in 31 PLADs and Xinjiang Production and Construction Corps (XPCC) of the mainland of China between 2011 and 2016, and the final effectiveness evaluation was conducted by a random sample survey in 347 hospitals.
¶ The third stage of NRP was launched in 31 PLADs and XPCC of the mainland of China between 2017 and 2021, and the effectiveness evaluation was based on surveillance data of all secondary and tertiary MCH institutions. The surveillance data were collected from the MCH institutions surveillance system of the National Center for Women and Children’s Health, China CDC.Table 1. Trends in asphyxia incidence and mortality rate during 2003‒2008, 2010‒2014, and 2017‒2020.
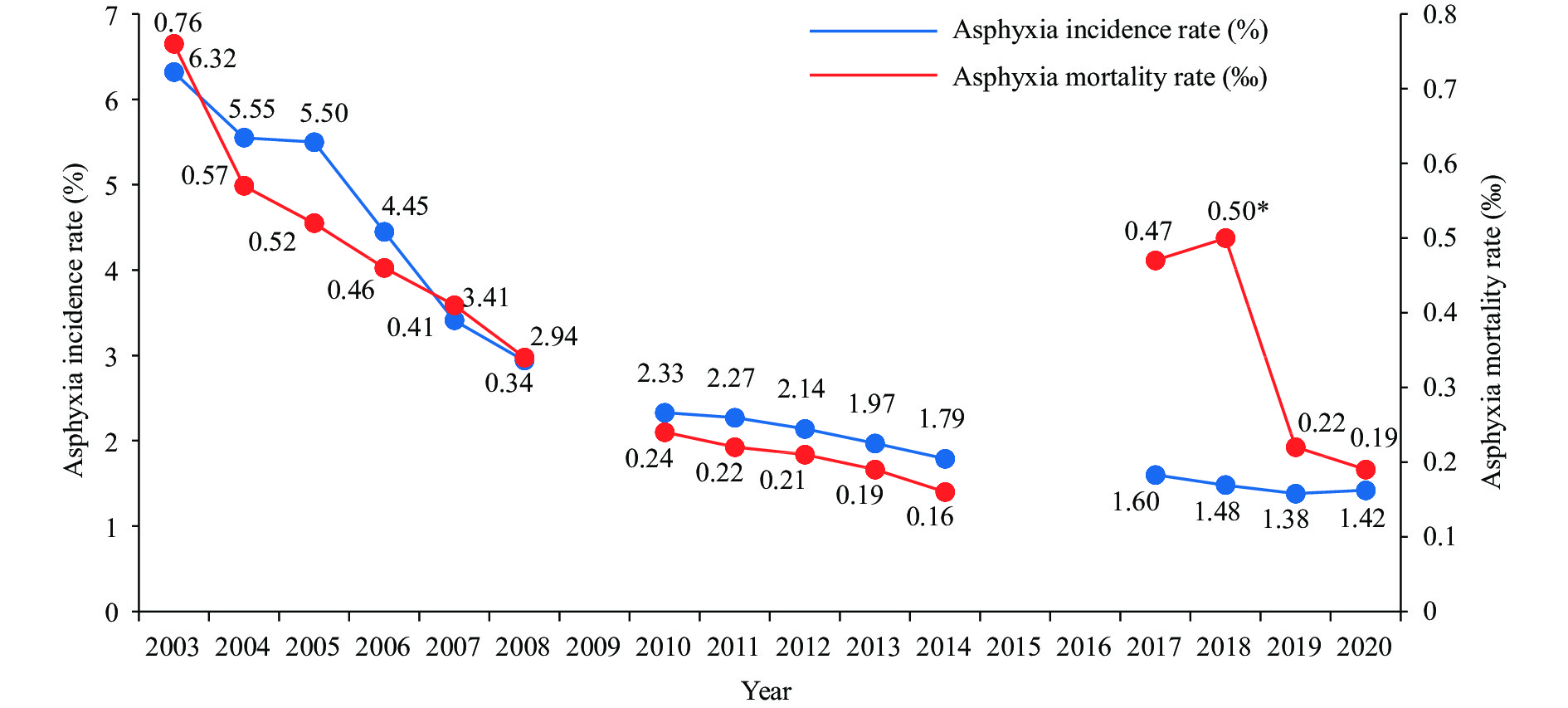 Figure 1.
Figure 1.Trends of neonatal asphyxia incidence and mortality rate in China, 2003‒2020.
Note: Data from 2003‒2008, 2010‒2014, and 2017‒2020 were obtained from a random sample survey in 322 hospitals, a random sample survey in 347 hospitals, and the surveillance data of all secondary and tertiary MCH institutions, respectively.
Abbreviation: MCH=maternal and child health.
* The abrupt increase in asphyxia mortality rate in 2017 and 2018 may be associated with the increased proportion of pregnant women of advanced maternal age (>35 years) after the implementation of the “universal two-child policy” released in October 2015.
-
To reduce neonatal mortality, relevant health authorities, academic associations, and social welfare organizations have reached a consensus and provided human, material, and financial support to form a stable and efficient programme management mechanism. China developed local technical guidelines for neonatal resuscitation and strengthened health staff clinical operational skills through theoretical education combined with simulated demonstrations. By building training teams through cascaded training, neonatal resuscitation techniques were mastered in a relatively short period of time. Evidence has shown that neonatal resuscitation techniques mitigate early birth asphyxia-attributable disease burden and yield favorable economic benefits (8). One pooled study conducted in low- and middle-income countries suggested that standardized formal neonatal resuscitation training decreased early neonatal mortality [relative risk (RR): 0.85, 95% CI: 0.76–0.96] (10). Practical experience gained from NRP has been translated into national policy, thus providing solid institutional support for sustainable application. Further implementation is warranted to promote well-being of neonates. However, potential challenges exist, such as the lack of available resuscitation equipment, adherence to resuscitation techniques for trainees, and periodic quality supervision of technical training. Specifically needed for improved neonatal survival are concerted efforts to promote practical skills in health facilities at the county level and below, establishment of an effective mechanism for monitoring and evaluation, and enhancement of coordination among multiple partners (8). In response to the goal to promote neonatal health in the 14th Five-Year Health Development Plan and Healthy China 2030, further implementation of neonatal resuscitation is necessary to put core principles into practice (11).
-
No conflicts of interest.
HTML
Multiple Parties Work in a Government-led Management Mechanism
Cascading Neonatal Resuscitation Training
Supportive Policy Environment for Sustainable Implementation
| Citation: |




 Download:
Download:




