-
Myanmar has made significant progress in reducing malaria morbidity and mortality. Plasmodium vivax (P.v) malaria is prevalent in 291 out of 330 townships in Myanmar. The annual parasite index (API) of malaria cases has decreased significantly in Myanmar, with a reduction from 10.00 to 1.46 cases per 1,000 population between 2009 and 2018, marking an 85.40% decline. Malaria detection and management services are available at public health facilities and village levels, administered by volunteers. There is a notable variance in malaria incidence between the western and eastern regions of Myanmar. Transitioning from malaria control to elimination poses challenges. This study aims to assess the gaps in National Malaria Control Programme (NMCP) services at community, township, and national levels. It will provide action plans and policy recommendations based on the analysis of malaria incidence and prevalence in hotspot areas of Rakhine State.
HTML
-
The aim of this research is to assess the current status and effectiveness of the intensified plan aimed at reducing malaria cases in high-risk townships in Myanmar.
-
To analyze the malaria situation, including the annual blood examination rate (ABER) and API, from 2015 to 2020.
To analyze the intensification plan activities in the malaria hotspot area from 2017 to 2020 (1).
To evaluate the impact of the integrated community health care service intervention in the Minbya Township hotspot area, Rakhine State.
-
The study utilized a surveillance design to examine epidemiological trends in communicable and tropical diseases, with a specific focus on malaria in high-incidence townships in the northern regions of Rakhine State. This design encompassed the systematic gathering and observation of health data for investigating outbreak response patterns. The research targeted the entire population of Minbya Township in Rakhine State over the period from 2015 to 2020. We established inclusion criteria to ensure data variability and reliability. The criteria encompassed residents of Minbya Township afflicted with malaria between 2015 and 2020 as well as local volunteers working with the NMCP as village health volunteers (VHVs). Secondary data on malaria P&C services, including annual records of tested and confirmed malaria cases (Plasmodium falciparum, Plasmodium vivax, and mixed infections), were utilized from the malaria surveillance system (MSS) (2) and the township-level Malaria-Related Hotspot Area Reporting databases for the years 2015–2020. Additionally, the WHO’s malaria monitoring dashboard for Minbya Township was employed to identify seasonal patterns and high-risk transmission zones, drawing from data provided by six rural health centers (RHCs) (3). The study aimed to identify contributory factors to the observed reduction in malaria burden and to discuss the intensified control strategies that have played a role in decreasing the malaria disease burden in Myanmar.
-
The epidemiological analysis relies on factors such as disease transmission, susceptibility, health services, and population behavior. The malaria surveillance database provides insights into the population’s mobility, mortality trends, and the number of tested and positive malaria cases from 2015 to 2020, as shown in the Table 1 below.
Year Population ABER API Tested Positive 2015 210,072 8.36 13.34 17,569 2,804 2016 215,294 6.27 8.85 13,519 1,906 2017 220,431 11.28 8.26 24,869 1,821 2018 222,412 8.58 6.06 19,089 1,359 2019 228,191 7.40 3.46 16,900 790 2020 230,605 5.42 2.25 12,366 514 Abbreviation: ABER=annual blood examination rate; API=annual parasite index. Table 1. Malaria prevalence in Minbya Township (2015–2020), Rakhine State.
The population of Minbya Township fluctuates between 210,072 and 230,605 individuals, with a mean of 221,167.5 due to population growth. Since 2017, the NMCP has enacted a strategy to enhance testing capacity and expand the involvement of VHVs. The API exceeded 1 per 1,000 people in seven townships in Rakhine state, falling short of the national strategic plan goal to reduce API to less than 1 per 1,000 by 2020. This collaboration has enabled the scaling up of capacity building in data management and reporting systems through the use of the malaria surveillance database at the township level. 3,857 local malaria volunteers have been trained since 2013 to support malaria elimination efforts. The NMCP collaborates with local partners to provide malaria prevention and control activities. Since 2017, 201 local malaria volunteers have been recruited and trained in malaria diagnosis and treatment guidelines as part of the malaria elimination plan. Among the VHVs, URC consistently provides 74 volunteers, comprising 112 males and 82 females. Two-thirds of the VHVs have obtained secondary education.
Table 2 displays the distribution of malaria species in Minbya Township from 2015 to 2020. Notably, there were no reported outbreaks of P.v during this period. Data from the malaria epidemiology monitoring dashboard of Minbya Township indicates that Plasmodium vivax species accounted for 55 percent, Plasmodium falciparum species for 42 percent, and the remaining cases involved mixed species.
Year % of Plasmodium falciparum % of Plasmodium vivax % of Mixed 2015 26 69 5 2016 21 75 4 2017 55 42 3 2018 43 55 2 2019 62 34 4 2020 43 52 5 Table 2. Percentage of malaria species in Minbya Township from 2015 to 2020.
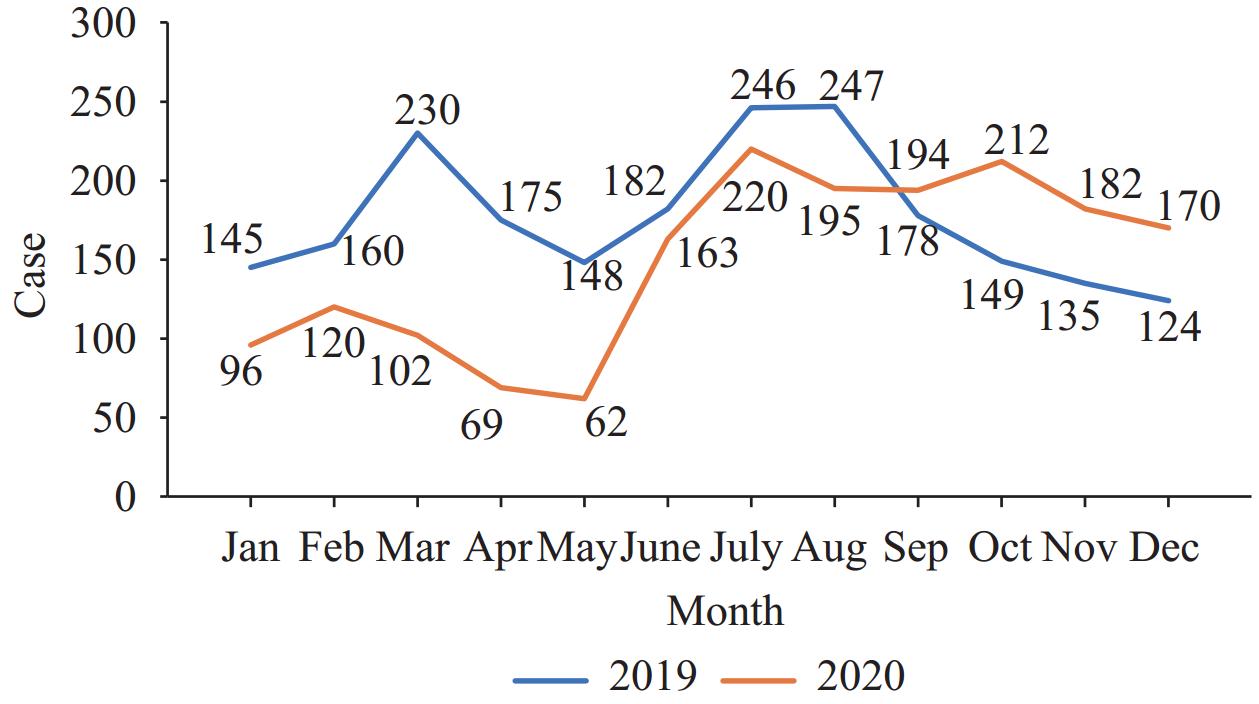
Figure 1 illustrates the comparison of malaria testing capacity in Minbya Township between 2019 and 2020. The capacity was assessed by basic health staff at healthcare centers like RHCs and sub-centers, excluding data from local malaria volunteers. In 2019, 2,119 patients were tested by basic health staff. From January to August, testing capacity was consistent, but it decreased from September to December. In 2020, 1,785 patients were tested, with reduced testing capacity from January to May, followed by an increase from May to December due to a seasonal disease prevention approach. This study indicates that the health care management by basic health staff has maintained an effective and timely reporting system. To prevent underreporting of malaria cases in 2020, the Basic Health Staff (BHS) conducted malaria testing alongside fever surveillance for coronavirus disease 2019 (COVID-19) (4). At the village level, detection capacity primarily relies on local community volunteers who provide integrated malaria services in their own and neighboring villages. They promptly test villagers with suspected COVID-19 symptoms like fever following the NMCP guidelines (5).
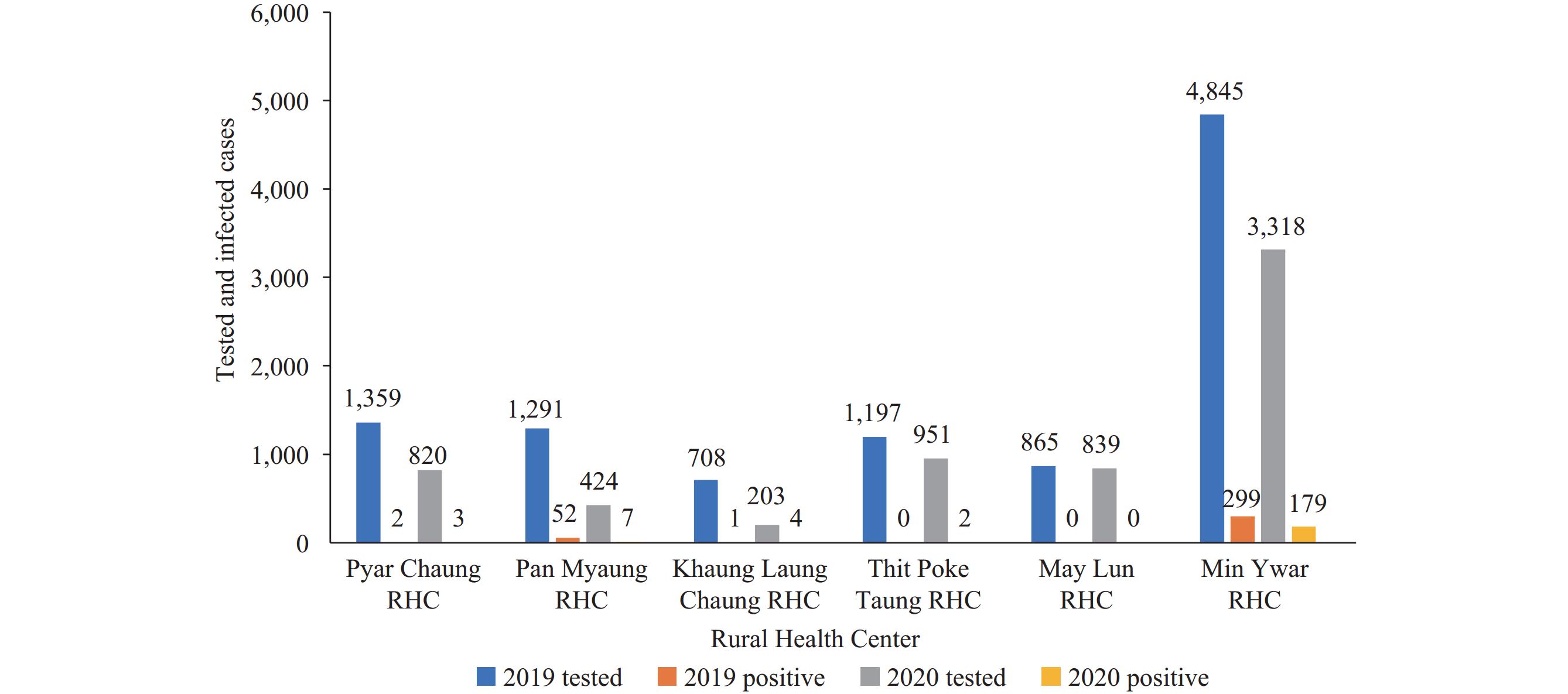
Figure 2 displays the number of malaria cases tested and confirmed in Minbya Township from 2019 to 2020 across six rural health centers (RHCs). Min Ywar RHC and Pan Maung RHC exhibit the highest prevalence of malaria due to factors such as geographical location and the increased vulnerability of certain populations, like forest workers and farmers, to malaria.
-
The study found that since 2017, integrated community health services have been enhanced by implementing active case detection, malaria diagnostics, and treatment facilitated by village health volunteers. Even though the annual blood examination rate declined significantly from 8.4 to 5.2 per 1,000 API, from 3 in 2015 to 2.5 in 2020, P&C measures such as active case detection and passive case detection and treatment have consistently helped reduce the number of malaria cases, from 2,804 in 2015 to 514 in 2020. The incidence of malaria is associated with specific occupation types and affects vulnerable populations (6). Amid the COVID-19 pandemic, the rapid diagnostic testing capacity remained a critical component of malaria prevention programs, especially given movement restrictions. Furthermore, there was no decline in malaria testing capacity due to the effective coverage provided by community health volunteers in their villages during 2020. Data on malaria-positive cases and testing from various villages are invaluable for analyzing transmission stratification, thereby facilitating the targeted implementation of intensified plan activities. At the community level, detection capabilities are largely attributed to local volunteers, who reside within and serve surrounding villages, offering integrated malaria services. This proximity allows immediate access to medical treatment and RDT for villagers exhibiting COVID-19-related symptoms such as fever, in alignment with NMCP guidelines. In 2019, populations at risk, residing in areas with high malaria transmission within this township, received long-lasting impregnated bed nets (LLINs) (7), encouraging local utilization and sense of ownership. LLINs have proven to be an extremely effective measure for preventing contact between human and vectors. It is recommended that implementing early detection strategies and promoting treatment in hotspot areas of townships with high malaria prevalence should be part of a comprehensive approach to reducing the disease burden under an integrated intensification plan of the NMCP (8). This research finding will support the sustainable action plan for community-based health service activities in the hotpot area after the intensification plan completion. However, it may have some limitations as follows;
1) it is needed to upgrade the national strategic plan for meaningful advocacy engagement of the civil society and private actors in the malaria surveillance system (MSS) including infodemic risk mitigation plan.
2) the political crisis and shortage of human resources such as vector-borne disease control townships’ focal person;
3) weakness of technical skills for digital technology management problem of health information management system (health management and information system and district health information system complexity), also our data was only collected from one hotspot township, and the time was in 2020–2021. As a suggestion, we would like to have more years of reliable data on townships that engage in malaria control and prevention activities, to evaluate the impact and sustainability of the mentioned public health countermeasure (9). Therefore, a reliable, innovative, and advanced technology surveillance approach is needed in the future and will be expanded to other hotspot townships during further pandemics. It is concluded that focusing on the malaria elimination strategy and implementation plan for the highly epidemic areas in Myanmar supports further research cooperation for digital-based real-time malaria surveillance which carries out epidemiological analysis of its associated factors among the Greater Mekong Subregion countries (10).
No conflicts of interest with others or potential funding for this research study.
| Citation: |



 Download:
Download: