-
Malaria, caused by Plasmodium spp., remains a significant life-threatening infectious disease globally. The World Health Organization (WHO) reported 608,000 malaria-related deaths and approximately 249 million cases in 2022 (1). Although China received WHO certification for malaria elimination on June 30, 2021, the country continues to report thousands of imported cases annually, and Anopheles mosquitoes, vectors of the disease, persist in formerly endemic regions. Consequently, China must continuously strive to maintain its malaria-free status (2–3). Historically, research in China has focused on the time from the onset of fever symptoms to the diagnosis in patients with imported malaria prior to the implementation of the “1-3-7” strategy (4–5). This three-tiered approach involves: 1) reporting cases within one day; 2) conducting case investigations within three days; and 3) initiating focus investigation and action within seven days (6). Data from 2014 to 2021 across five provinces have been analyzed to map the timeline of imported malaria cases from their arrival in China to treatment. This study aims to underpin preventative strategies against the re-establishment of malaria and to enhance health education for overseas arrivals in China.
Data on imported malaria cases from January 2014 to December 2021 were collected from Henan, Anhui, Zhejiang, Hubei, and Guangxi using the National Notifiable Disease Reporting System (NNDRS) and the Parasitic Diseases Information Reporting Management System (PDIRMS). An imported malaria case was defined as a malaria infection acquired outside China, diagnosed in either Chinese or foreign residents within the country. The recorded data included variables such as age, gender, Plasmodium species, infection origin, severity, previous malaria infections, travel purpose, and relevant dates pertaining to the disease timeline — arrival in China, symptom onset, initial care-seeking, diagnosis, and treatment. Cases excluded from the study were those of indigenous malaria, imported secondary infections, relapses or recrudescence, and non-mosquito-borne transmissions, such as those acquired through blood transfusion or with incomplete information. The duration from the patient’s arrival in China to treatment was segmented into the following intervals: 1) arrival to symptom onset, 2) symptom onset to initial care-seeking, 3) initial care-seeking to diagnosis, and 4) diagnosis to treatment. This study specifically focused on the timeline from symptom onset to treatment, as antimalarial drug administration followed China’s National Guidelines per the Technical Regulations for Application of Antimalarials (WS/T 485-2016) (7). Continuous variables following a normal distribution were analyzed using means and standard deviations (SD), while those not normally distributed were described using medians and interquartile ranges (IQR). Categorical variables were evaluated using the chi-squared test, and time intervals between the four primary malaria species were examined through the nonparametric Kruskal-Wallis H test. A P-value of <0.05 was considered statistically significant. Furthermore, multiple comparisons between the four main Plasmodium species groups (P. falciparum, P. vivax, P. malariae, P. ovale) were assessed using the Bonferroni method with an adjusted significance level α set at 0.008 (0.05/6). Thus, P<0.008 was deemed statistically significant for these analyses. All analyses were performed using SPSS (version 21.0; SPSS, Inc., Chicago, US).
From 2014 to 2021, a total of 4,614 malaria cases from five Chinese provincial-level administrative divisions (PLADs) were analyzed. The average age of the patients was 40.04±9.62 years, with males comprising 97.18% (4,484 cases) of the total. The most common malaria species identified were P. falciparum, followed by P. ovale, P. vivax, P. malariae, and P. knowlesi. A significant majority of the cases (96.66% or 4,460) were contracted in Africa, with the remaining 3.06% (141) originating from Asia. Migrant workers accounted for 87.31% (4,028 of 4,614) of the imported cases. Of the total cases, 253 were classified as severe malaria, while 4,361 were considered non-severe. Additionally, 74.36% (3,431) had a history of malaria infection abroad (Table 1).
Characteristics Number (%) Age, years (mean±SD) 40.04±9.62 Sex, n (%) Male 4,484 (97.18) Female 130 (2.82) Plasmodium species Plasmodium falciparum 3,206 (69.49) Plasmodium vivax 313 (6.78) Plasmodium ovale* 887 (19.22) Plasmodium malariae 138 (2.99) Plasmodium knowlesi 1 (0.02) Mixed infections 69 (1.50) Infection sites Africa 4,460 (96.66) Asia 141 (3.06) Others 13 (0.28) Travel purpose Migrant work 4,028 (87.31) Business 276 (5.98) Official duties 206 (4.46) Others 104 (2.25) Severe malaria Yes 253 (5.48) No 4,361 (94.52) History of malaria infection Yes 3,431 (74.36) No 1,183 (25.64) Abbreviation: SD=standard deviation.
* contains the number of subtypes of ovale malaria.Table 1. Epidemiological characteristics of 4,614 imported malaria cases in China, 2014–2021.
In a study of 4,614 malaria patients, 214 (4.64%) exhibited symptoms before arriving in China, 3,313 (71.80%) developed symptoms within one month of arrival, 4,593 (99.54%) sought healthcare within that same timeframe, and 4,597 (99.63%) were diagnosed within a month. Among 3,206 P. falciparum patients, 2,842 (88.65%) presented symptoms within a month, 3,191 (99.53%) sought medical attention within a month, and 3,200 (99.81%) were diagnosed promptly within this period. For the 313 P. vivax patients, 120 (38.34%) showed symptoms within a month, 310 (99.04%) sought healthcare within a month, and two (0.64%) sought medical help after three months, with no cases delayed beyond six months. Among 138 P. malariae patients, 68 (49.28%) exhibited symptoms within a month, all sought healthcare within this period, and 98.55% were diagnosed within a month, with no diagnoses extending past three months. For 887 P. ovale patients, 236 (26.61%) showed symptoms within a month, 885 (99.77%) were diagnosed within a month, and seven (0.79%) were treated after a month (Figure 1).
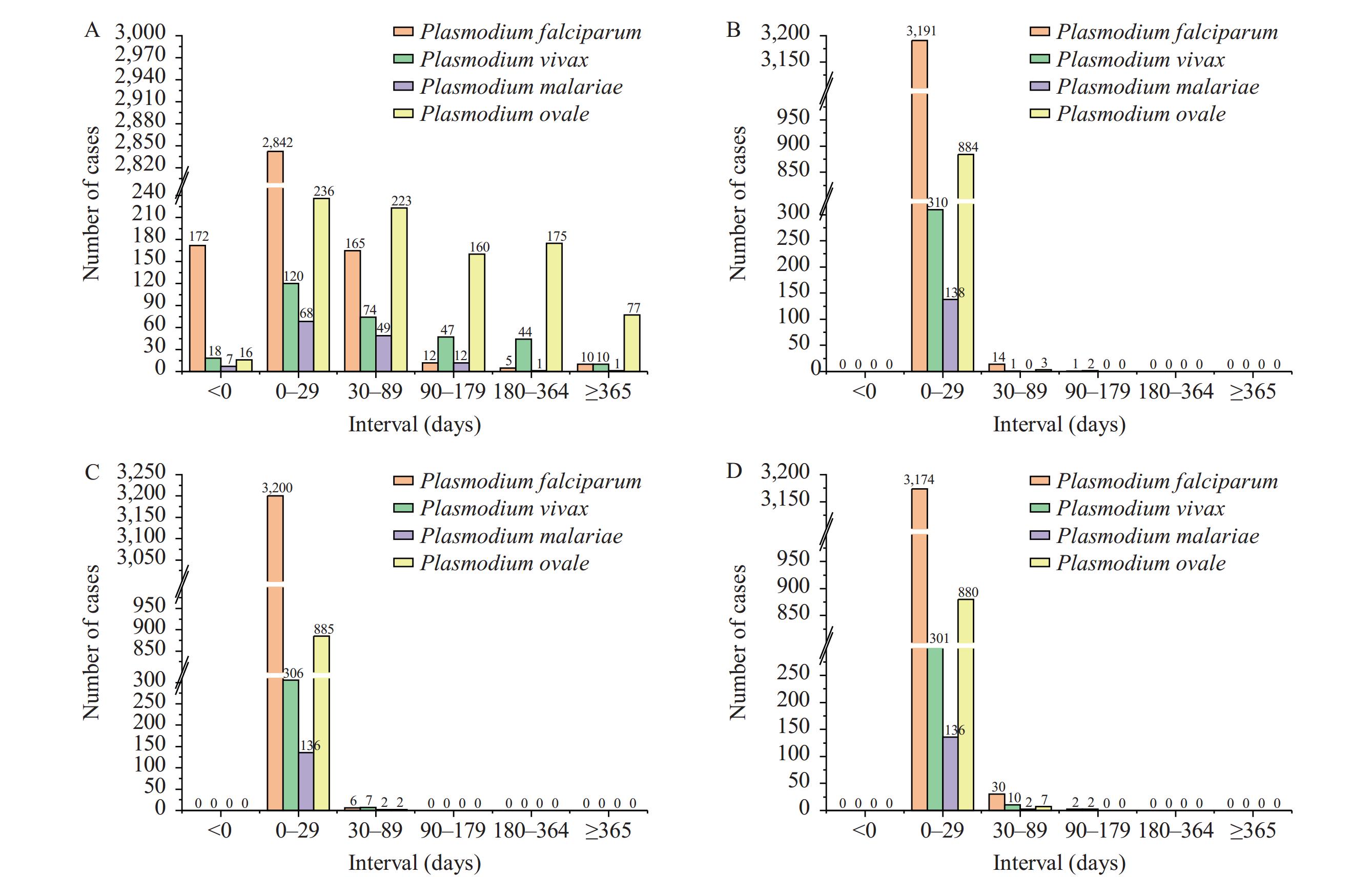 Figure 1.
Figure 1.Number of patients for four malaria species from arrival in China to treatment. (A) Time from arrival in China to symptom onset; (B) time from symptom onset to initial care-seeking; (C) time from initial care-seeking to diagnosis; (D) time from symptom onset to treatment.
As shown in Table 2, the median time interval from arrival in China to symptom onset was 9 days for all malaria species, with an IQR of 3 to 27 days. The median time from symptom onset to initial care-seeking was 1 day (IQR: 0–2 days). The median duration from initial care-seeking to diagnosis was 0 days (IQR: 0–2 days), and from symptom onset to treatment was 2 days (IQR: 1–4 days). Statistically significant differences were noted among the four main malaria species (P<0.001). Specifically, for the interval from arrival to symptom onset, the longest median and IQR were observed for P. ovale at 78 days (24–202 days), followed by P. vivax at 42 days (12–128 days), P. malariae at 24.5 days (11–49 days), and P. falciparum at 6 days (2–6 days) (P<0.008). For the interval from symptom onset to initial care-seeking, P. vivax was 1 day (0–3 days) and P. malariae was 1.5 days (0–4 days), which was longer than P. falciparum at 1 day (0–2 days) (P<0.008). For the interval from initial care-seeking to diagnosis, significant differences were observed among P. falciparum (0 day, IQR: 0–1.75 days) vs. P. vivax (0 day, IQR: 0–3 days), P. ovale (0 day, IQR: 0–1 day) vs. P. vivax, P. falciparum vs. P. malariae (1 day, IQR: 0–4 days), and P. malariae vs. P. ovale (P<0.008). Except for P. vivax vs. P. malariae, significant differences were recorded in the intervals between symptom onset and treatment (P<0.008). The time intervals for P. malariae (4 days, IQR: 2–8.75 days) were longer than those for P. falciparum (2 days, IQR: 1–4 days) and P. ovale (2 days, IQR: 1–5 days).
Time intervals Plasmodium falciparum Plasmodium vivax Plasmodium ovale Plasmodium malariae Total* H† P-value N M
(IQR)N M
(IQR)N M
(IQR)N M
(IQR)N M
(IQR)Interval between arrival in China and symptom onset 3,206 6
(2–11)313 42§,***
(12–128)887 78¶,**,***
(24–202)138 24.5††,§§,¶¶,*** (11–49) 4,614 9
(3–27)1,417.036 <0.001 Interval between symptom onset and initial care-seeking 3,206 1
(0–2)313 1§,***
(0–3)887 1
(0–3)138 1.5††,***
(0–4)4,614 1
(0–2)24.324 <0.001 Interval between initial care-seeking and diagnosis 3,206 0
(0–1.75)313 0§,***
(0–3)887 0**,***
(0–1)138 1††,¶¶,***
(0–4)4,614 0
(0–2)28.606 <0.001 Interval between symptom onset and treatment 3,206 2
(1–4)313 3§,***
(1–7)887 2¶,**,***
(1–5)138 4††,¶¶,***
(2–8.75)4,614 2
(1–4)103.829 <0.001 Note: Unit: days.
Abbreviation: M=median; IQR=interquartile range.
* contains P. knowlesi and mixed infections; † means the four main malaria species were compared; § compares the P. falciparum group with the P. vivax group; ¶ compares the P. falciparum group with the P. ovale group; ** compares the P. vivax group with the P. ovale group; †† compares the P. falciparum group with the P. malariae group; §§ compares the P. vivax group with the P. malariae group; ¶¶ compares the P. ovale group with the P. malariae group; *** indicates statistically significant differences.Table 2. Duration between arrival in China and initiation of treatment for imported malaria cases, 2014–2021.
-
The study revealed that the median duration from arrival in China to the onset of symptoms varied across Plasmodium species: 9 days for all species combined, 78 days for P. ovale, 42 days for P. vivax, 24.5 days for P. malariae, and 6 days for P. falciparum. Notably, the maximum duration reached 1,860 days for P. ovale and 1,225 days for P. vivax. Such extended periods may lead patients to overlook their history of international travel. The median duration from symptom onset to the first medical consultation was 1 day for all malaria cases. However, except for P. malariae, for which the median duration was also 1 day, the time from first healthcare-seeking to diagnosis was immediate (0 days) in this study. These findings slightly deviate from those reported in a previous study, which observed median durations of 3 days from fever onset to healthcare-seeking and 2 days from healthcare-seeking to diagnosis (4). The discrepancy might be due to the relatively low number of malaria cases (90 cases) included from Shanxi Province, potentially affecting the outcomes. P. falciparum cases demonstrated a shorter duration between symptom onset and treatment initiation than the other three Plasmodium species, with P. malariae showing the longest duration (4 days). This variation could be attributed to interactions among P. malariae and P. ovale with co-infections of P. falciparum and P. vivax in regions where these last two species predominate, leading to frequent underdiagnosis of the former species (8). Additional studies have indicated median intervals between onset and diagnosis of 4 days (IQR: 2–7 days) in Henan Province during 2010–2017. In Yunnan Province, where there is significant mobility of the migrant population along the China-Myanmar border, the duration was longer, averaging 5.1 days (9-10).
The primary limitations of this study are twofold. First, the inclusion of a limited number of PLADs may not adequately represent the time intervals between entry into China and subsequent treatment. Second, the time intervals between the onset of illness and treatment could have been influenced by the coronavirus disease 2019 (COVID-19) period.
In summary, P. falciparum is characterized by a shorter interval between arrival in China and symptom onset, as well as between symptom onset and treatment initiation, compared to the other three Plasmodium species. P. ovale and P. vivax typically have extended periods from arrival to symptom onset, though the duration from symptom onset to treatment commencement is brief. Conversely, P. malariae demonstrates a shorter timeline from arrival to symptom onset, with a prolonged period from symptom onset to treatment. It is crucial to provide malaria health education to overseas populations arriving in China, particularly from Africa and Southeast Asia, and to enhance diagnostic vigilance among physicians to increase the rate of timely diagnosis and prevent severe cases of malaria and fatalities.
-
No conflicts of interest.
-
We extend our gratitude to all participants who volunteered their time for this study.
HTML
| Citation: |



 Download:
Download:




