-
The incidence of human immunodeficiency virus (HIV) cases in young male students who had sex with men (MSM) has reported an average annual 10% increase in HIV diagnoses from 5,841 in 2010 to 13,717 in 2019 in China (1). The rise and popularity of geo-social networking apps used by young MSM (YMSM) have a parallel increased risk for sexually transmitted infections (STIs), due to an increase in the number of partners and a reduction in sexual health behaviors (2). However, lowering community viral load through treatment as prevention (TasP) (3) has become a critical HIV response strategy, by reducing sexual transmission among persons living with HIV (PLHIV) (4). In this paper, we sought to describe and examine the association and magnitude of social contacts within the social network of an app that employs serosorting to identify the uneven social linkage among college MSM in Northeast China. In this study, we recruited 759 college MSM and 382 of their social contacts from the Yiyou app from April 2017 to June 2018. A total of 98 participants (8.6%) were confirmed HIV positive during baseline and follow-ups serology tests, of whom 34 were college MSM. For college MSM, HIV positive prevalence at baseline and incidence at follow-ups were 3.8% (29/759) and 2.9 per 100 person-years (PY) (5/170.50 PY). Network graphing visualization showed that HIV-positive MSM had comparatively more social contacts (social dynamic) than the seronegative MSM. Therefore, identifying certain individuals as hyper-linkages within college MSM social network can inform tailored HIV prevention strategies such as sending reminders for information about antiretroviral therapy (ART) and promoting safer sexual behaviors.
We conducted a prospective longitudinal study and recruited participants among Yiyou app (developed by Heilongjiang Kangtong Community [HKC]) users. HKC manages 21 offline voluntary counseling and testing (VCT) sites using the Yiyou app umbrella in 16 cities within Northeast China to facilitate serosorting and other offline services, by appointment. The Yiyou app users must register with a cell phone number that is later used to share testing information with a mutual agreement upon inquiry, i.e., partner informed serosorting purposes (Figure 1A). That is the main reason for the app’s popularity. We recruited participants via three methods, including online advertisements on the Yiyou app homepage, person-to-person sharing by HKC visitors, and public service announcements in offline VCT clinics of HKC. The participants’ recruitment and follow-up procedures were detailed in Figure 1B. A self-administered structured questionnaire was conducted via the Yiyou app on sociodemographic information, perceived risk of HIV infection, sexual behaviors, recreational drug use in the past 6 months, and HIV self-testing experience. Upon completion of the online survey, participants were asked to undertake dual rapid HIV and syphilis tests and a parallel rapid HIV test by trained workers in offline VCT sites and confirmed HIV testing at a provincial CDC. Descriptive analyses were performed to identify the distribution of sociodemographic and behavioral characteristics and a Mann–Whitney U test was used to identify the difference in number of social contacts between the two HIV statuses.
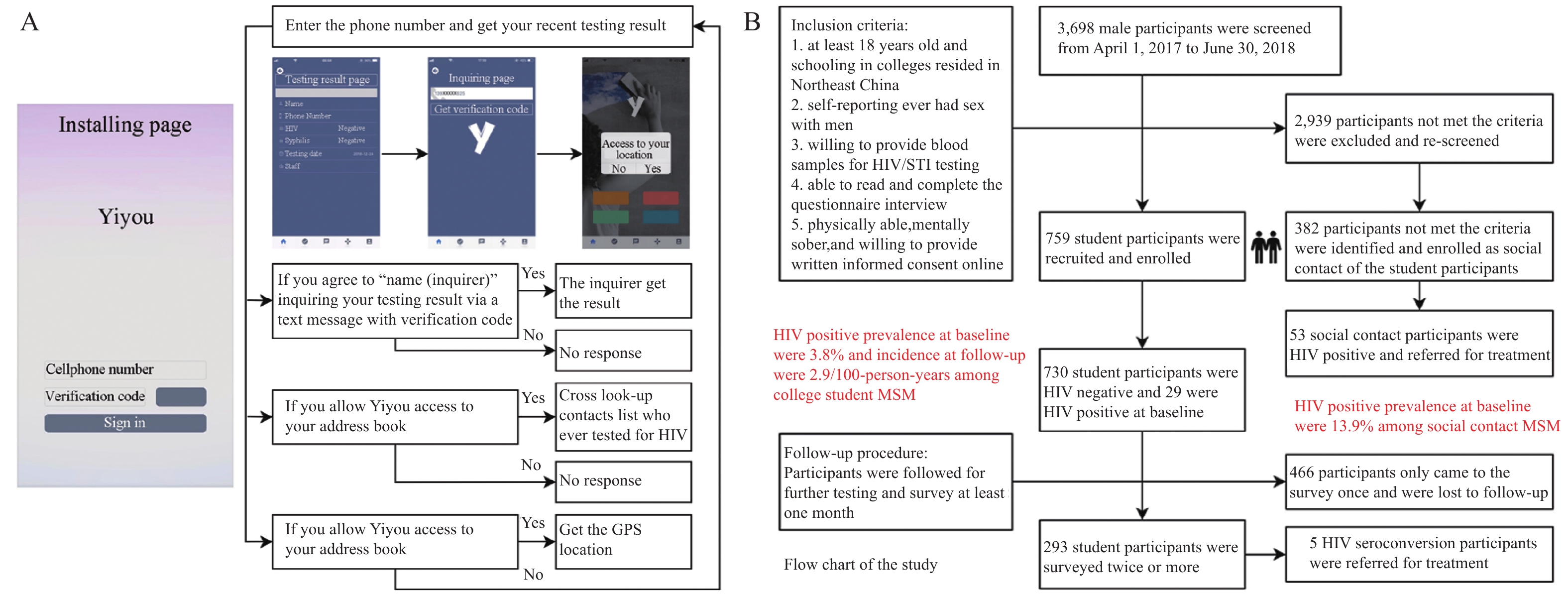 Figure 1.
Figure 1.Illustration and flowchart of the study. (A) The illustration of Yiyou App installation and use process; (B) The flowchart of participants' recruitment and follow-up procedure of the study.
Abbreviation: HIV=human immunodeficiency virus; STI=sexually transmitted infection.As per informed consent, we enhanced the Yiyou app information with a social parameter, using latitude and longitude from GPS data of all universities in Northeast China to verify the students’ identity by their geolocation sign-in, in addition to self-reported student identity. After a predesigned de-identification procedure, contact lists were linked to registered users of the Yiyou app and the social contacts were filtered by logical inference from the label information of phone contacts. Furthermore, we calculated the number of social contacts for each participant and determined the linkage for each participant as a snapshot of the whole social network at the end of the study, midnight of June 30, 2018. We used network analytic techniques to provide a “snapshot” to characterize what the network looks like as a static social structure. Nodes represent users and links represent interactions between users; the size of the node is proportional to the number of social contacts. The algorithm finds each node by minimizing the dispersion of the whole system. Microsoft Excel (Microsoft®, Albuquerque, New Mexico, USA) and Statistical Analysis System (Version 9.4, SAS Institute Inc., Cary, North Carolina, USA) were used to manage the dataset and conduct analyzes and Gephi® software for Windows (V.0.9.2) was used to visualize the social network.
Of 3,698 persons approached, 1,141 (30.9%) became study participants aged 24 years old [interquartile range (IQR)=21–33]; 759 (66.5%) were college student and 382 (33.5%) non-student contacts. A total of 98 participants (8.6%) were confirmed HIV positive during baseline and follow-ups, of whom 34 were college MSM. For college MSM and their social contacts, HIV prevalence at baseline and incidence in follow-ups were 3.8% (29/759) and 2.9 per 100 PY (5/170.50 PY), 13.9% (53/382), and 10.5 per 100 PY (11/105.06 PY), respectively.
Among college MSM, 97% were Han ethnicity, 96% were not married to a woman, 44.3% were migrants without local residency permits (hukou), 61.7% lived in Northeast China for >2 years, and 75.6% self-identified as homosexual. Regarding risk perception and sexual behavior, 29.8% perceived their risk of HIV infection as moderate or high. In the past 6 months, 49.5% reported anal sex, 47.6% used condoms consistently, 25.8% had >1 regular partners, and 18.3% used recreational drugs (Table 1). The median number of social contacts of college students was zero compared to two of their social contacts. The number of social contacts showed a significant difference (Z=6.1, P<0.001) between 98 HIV positive MSM (median: 1, IQR: 1–2) and 1,043 HIV negative MSM (median: 0, IQR: 0–1).
Factors College students, n=759 Social contacts, n=382 Total, N=1,141 n (%) n (%) n (%) Age (years)* Median 22 33 24 IQR 20–26 26–47 21–33 Ethnic Han 736 (97.0) 370 (96.9) 1,106 (96.9) Minority 22 (2.9) 8 (2.1) 30 (2.6) Marital status Married 25 (3.3) 47 (12.3) 72 (6.3) Unmarried 729 (96.0) 334 (87.4) 1,063 (93.2) Residence Local 422 (55.6) 254 (66.5) 676 (59.2) Other cities/PLADs 336 (44.3) 128 (33.5) 464 (40.7) Time spent locally <12 months 126 (16.6) 42 (11.0) 168 (14.7) 12–24 164 (21.6) 56 (14.7) 220 (19.3) >24 months 468 (61.7) 284 (74.3) 752 (65.9) Sexual orientation Homosexual 574 (75.6) 271 (70.9) 845 (74.1) Heterosexual 17 (2.2) 8 (2.1) 25 (2.2) Bisexual 115 (15.2) 81 (21.2) 196 (17.2) Uncertain 52 (6.9) 22 (5.8) 74 (6.5) Perceived risk of HIV infection No-low 533 (70.2) 223 (58.4) 756 (66.3) Moderate 171 (22.5) 118 (30.9) 289 (25.3) High-very high 55 (7.3) 41 (10.7) 96 (8.4) Having anal sex in the past 6 months Yes 376 (49.5) 266 (69.6) 642 (56.3) No 330 (43.5) 116 (30.4) 446 (39.1) Condom use with male partners in the past 6 months† Never 23 (6.1) 16 (6.0) 39 (6.1) Sometimes 174 (46.3) 91 (34.2) 265 (41.3) Every time 179 (47.6) 158 (59.4) 337 (52.5) Number of regular partners in the past 6 months† 0 48 (12.8) 42 (15.8) 90 (14.0) 1 231 (61.4) 148 (55.6) 379 (59.0) 2 74 (19.7) 53 (19.9) 127 (19.8) ≥3 23 (6.1) 23 (8.6) 46 (7.2) Any recreational drug use in the past 6 months Yes 139 (18.3) 103 (27.0) 242 (21.2) No 619 (81.6) 279 (73.0) 898 (78.7) Ever had HIV self-test Yes 282 (37.2) 124 (32.5) 406 (35.6) No 424 (55.9) 257 (67.3) 681 (59.7) Syphilis status Negative 698 (92.0) 329 (86.1) 1,027 (90.0) Positive 60 (7.9) 51 (13.4) 111 (9.7) Not sure 1 (0.1) 2 (0.5) 3 (0.3) Number of social contacts* Median 0 2 0 IQR 0–0 1–3 0–1 HIV status Negative 725 (95.5) 318 (83.2) 1,043 (91.4) Positive 34 (4.5) 64 (16.8) 98 (8.6) HIV positive rate Baseline (%) 29 (3.8) 53 (13.9) 82 (7.2) Follow-up (per 100 PY) 5 (2.9) 11 (10.5) 16 (5.8) Abbreviation: PLADs=provincial-level administrative divisions; MSM=men who have sex with men; IQR=interquartile range; HIV=human immunodeficiency virus; PY=person-years.
* Age and number of social contacts are skewed distributions; hence, we present median and interquartile range.
† Total number is of men who had anal sex in the past 6 months. PY stands for person-years. When numbers do not add to the expected sample size, it means that some men did not answer a given question.Table 1. Demographic and behavioral characteristics of college students and their social contacts among MSM in Northeast China, 2017-2018 (N=1,141).
Figure 2 allows us to identify highly connected individuals (i.e., hyper-linkages) with different HIV statuses among college students and their social contacts. It showed that HIV-positive MSM had comparatively more social contacts than their seronegative counterparts. However, some of the HIV positive students showed no social contact or declined to share social contact with us. Therefore, they are dispersed outside.
 Figure 2.
Figure 2.Network graph of the young men who have sex with men in Northeast China, 2017–2018, categorized by HIV sero-status and social identity (college students and social contacts, N=1,141).
Note: Nodes represent users and links represent interactions between users; the size of the node is proportional to the number of social contacts.
Abbreviation: HIV=human immunodeficiency virus.
-
We used HIV testing services data from the offline VCT sites and innovative app-derived social network data to describe and identify the HIV-positive men as hyper-linkages among college MSM who used the Yiyou serosorting app in Northeast China. HIV-positive men had comparatively more social contacts than HIV-negative people, presenting disproportionately more hyper-linkages within the MSM social networks.
In recent years, MSM bear a disproportionate burden of new HIV infections in China, and YMSM aged 15–24 are the most vulnerable population. In our study, the HIV prevalence and incidence were estimated as 3.8% and 2.9 per 100 PY, respectively, among college MSM aged 22 years old. A 7-city cross-sectional survey reported that YMSM had a higher HIV incident infection (up to 5.4% per annum) compared to MSM who were older (5). The drastic increment of annual reported cases among YMSM, including many university students, has garnered attention from the Chinese government and society (1).
It is noteworthy that HIV-positive MSM had comparatively more social contacts than the seronegative MSM. Not surprisingly, YMSM typically get to know each other through mobile dating apps, and they would leave mobile phone numbers to social contact only if they choose to meet or intend to have further communication (6). YMSM may be more easily influenced by a social contact, particularly one who exhibits trust by disclosing his sexual orientation. To safeguard their privacy, some college MSM may have more social contacts outside of the school than with student peers (7). Most YMSM prefer to use online dating apps when seeking potential sexual partners and calculating risk of HIV transmission (8). Moreover, homophobia or related stigmatization may be a barrier to accessing HIV prevention knowledge, an obstacle overcome by LGTBQ-friendly social media (9). We noticed that some HIV positive college men had no social contacts during the study period. It is possible some students caught HIV earlier than the research app launched. Therefore, dating apps and other social media apps can be used as an important prevention platform, especially if artificial intelligence algorithms can enable more individually tailoring for intervention.
The major strengths of this study include the following: the participation rate (>30%), which is high compared to many other internet-based surveys with a representative sample of MSM users of social apps in the real world; and the innovative app-derived social networking data, which enabled us to explore social network utilization. Limitations of this study include the following: the social networks were limited in the Yiyou app users and these findings cannot be generalized to other LGTBQ-friendly dating apps; the cross-sectional social contact information does not permit ascertainment of the direction of the findings or confidence in causal pathways; and the social contact information is unavoidably biased towards a minimum estimate in terms of the number, density, or breadth of their sexual network, due to the complexity of technology and human interaction.
In the following stages of our ongoing studies, we will focus on the key population at high HIV transmission risk and send reminders for information about ART and promote safer sexual behaviors to tap into the potential of LGTBQ-friendly apps for HIV prevention.
-
No conflicts of interest.
-
The participants’ contact information sharing as well as critical comments from the reviewers.
HTML
| Citation: |



 Download:
Download:




