2022 Vol. 4, No. 48
This study reported the trends and analyzed the age-period-cohort effects on the incidence and mortality rates of cervical cancer in China.
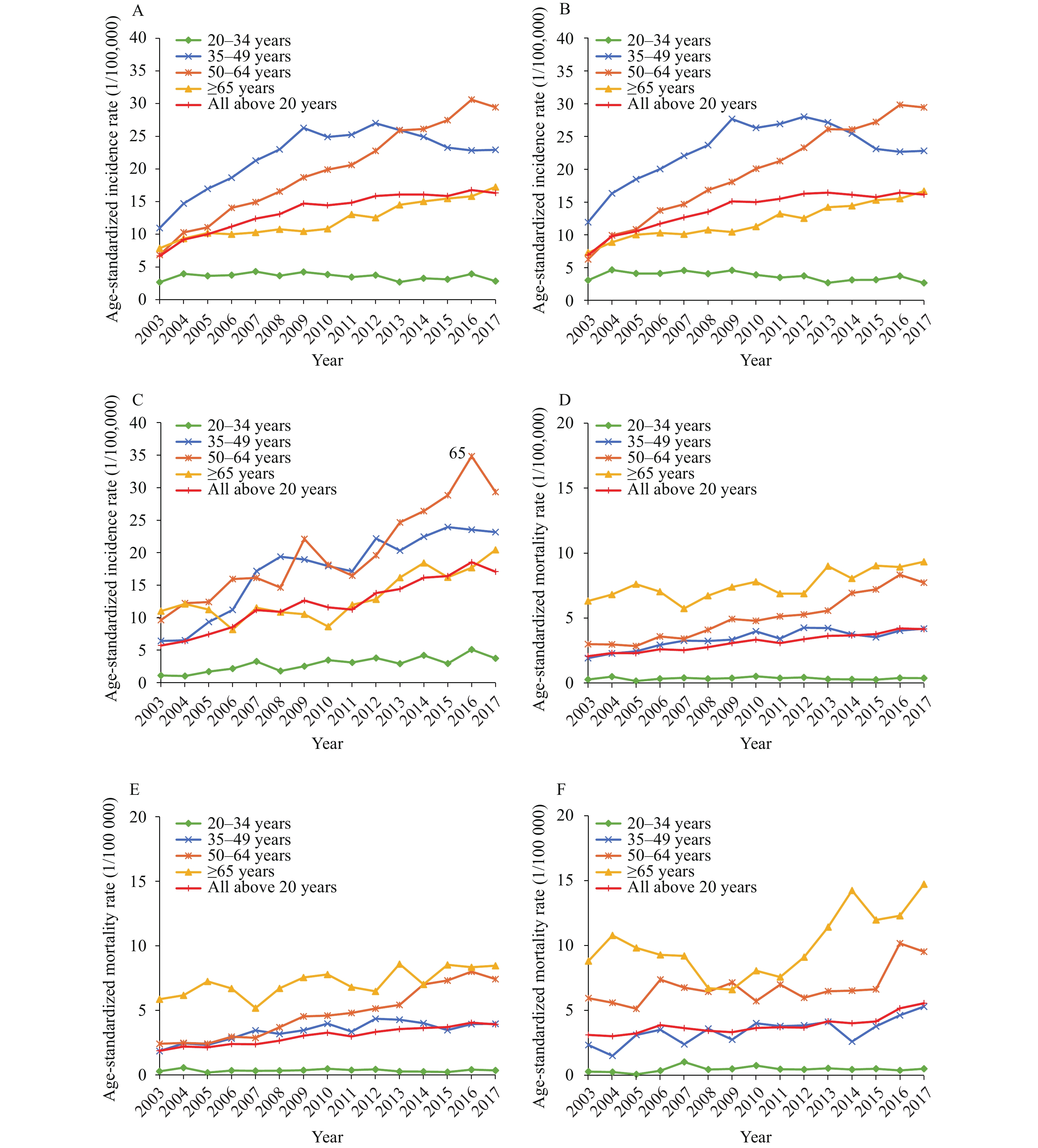
The age-standardized incidence rate (ASIR) and mortality rate (ASMR) by Segi’s world standard population were calculated using qualified consecutive data from 22 cancer registries from 2003 to 2017 in China. We performed joinpoint analysis to describe the trends and age-period-cohort analysis to estimate the independent effects of age, period and cohort on trends in incidence and mortality rates of cervical cancer.
The ASIR and ASMR for cervical cancer in females over 20 years old increased during 2003−2017. For females <50 years, a decreasing trend in ASIR and a stable trend in ASMR were observed in urban areas after 2009. But the ASIR and ASMR kept increasing in rural areas during the whole period. For females >50 years, the ASIR and ASMR increased both in urban and rural areas. Age-period-cohort analysis showed increasing period effects on cervical cancer incidence and mortality during the whole period. The cohort effects exhibited a downward-upward-downward pattern for the incidence (1918–1938, 1938–1963, 1963–1993) and mortality rates (1918–1943, 1943–1963, 1963–1993) in urban areas, a fluctuating pattern for incidence rate and a continuing downward pattern for mortality rate (1918–1993) in rural areas.
The increases in cervical cancer incidence and mortality rates can be mostly explained by period effects. We observed decreases in risk for cervical cancer incidence and mortality in young female generations, which were more obvious in urban areas.
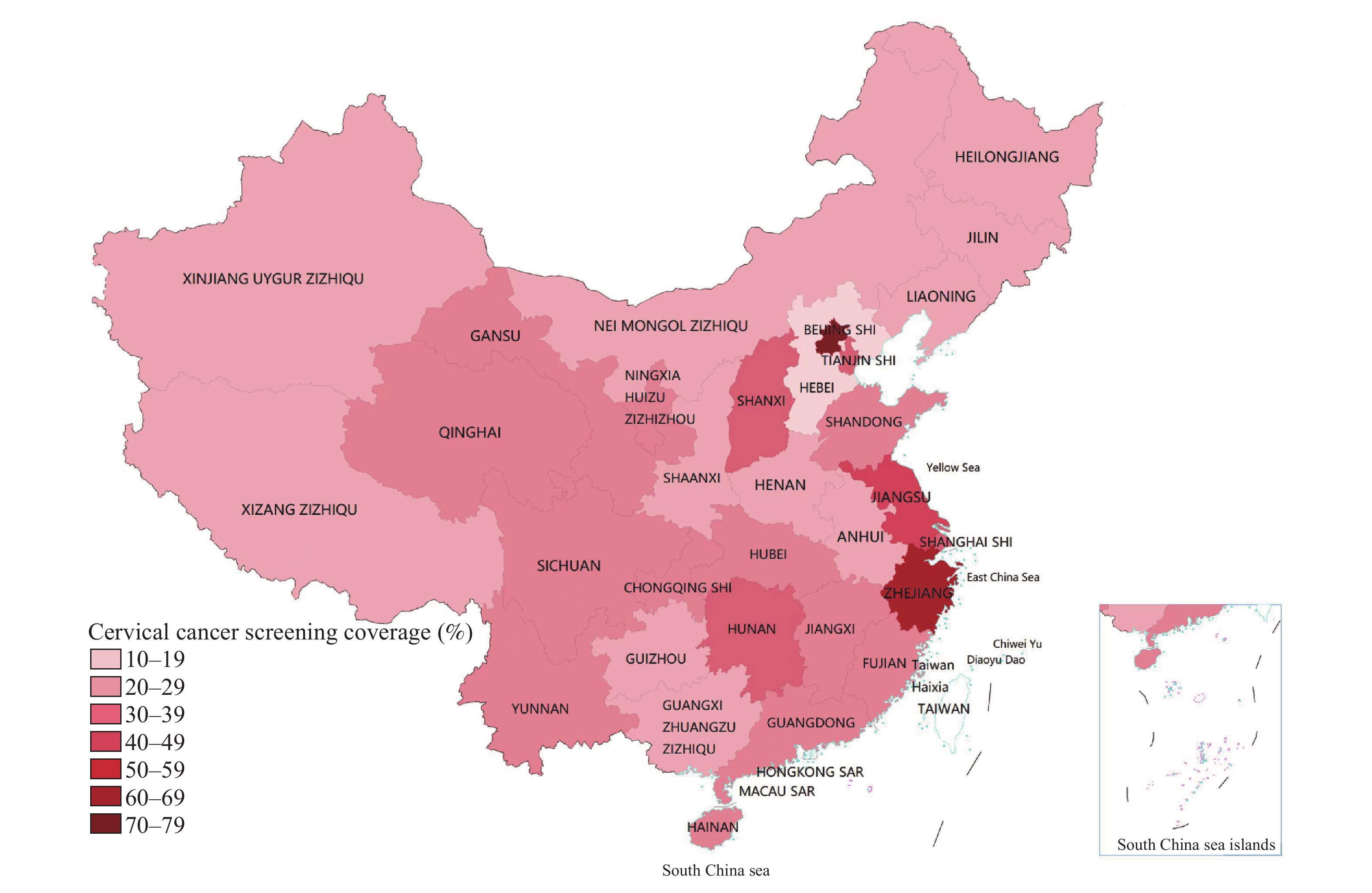
The World Health Organization set a 2030 target of 70% cervical cancer screening coverage for women aged 35–45 years. Coverage stood at 37% in China in 2015.
In 2018–2019, China’s cervical cancer screening coverage reached 43.4% in women aged 35–44 years and 36.8% in women aged 35–64 years. Screening coverage was still lower in rural areas as well as central and western regions; large variations existed across provincial-level administrative divisions.
National and local policy and financial support should be maintained for cervical cancer screening, along with more targeted health education and outreach efforts and strengthened accessibility of health services in the rural areas and central and western regions.
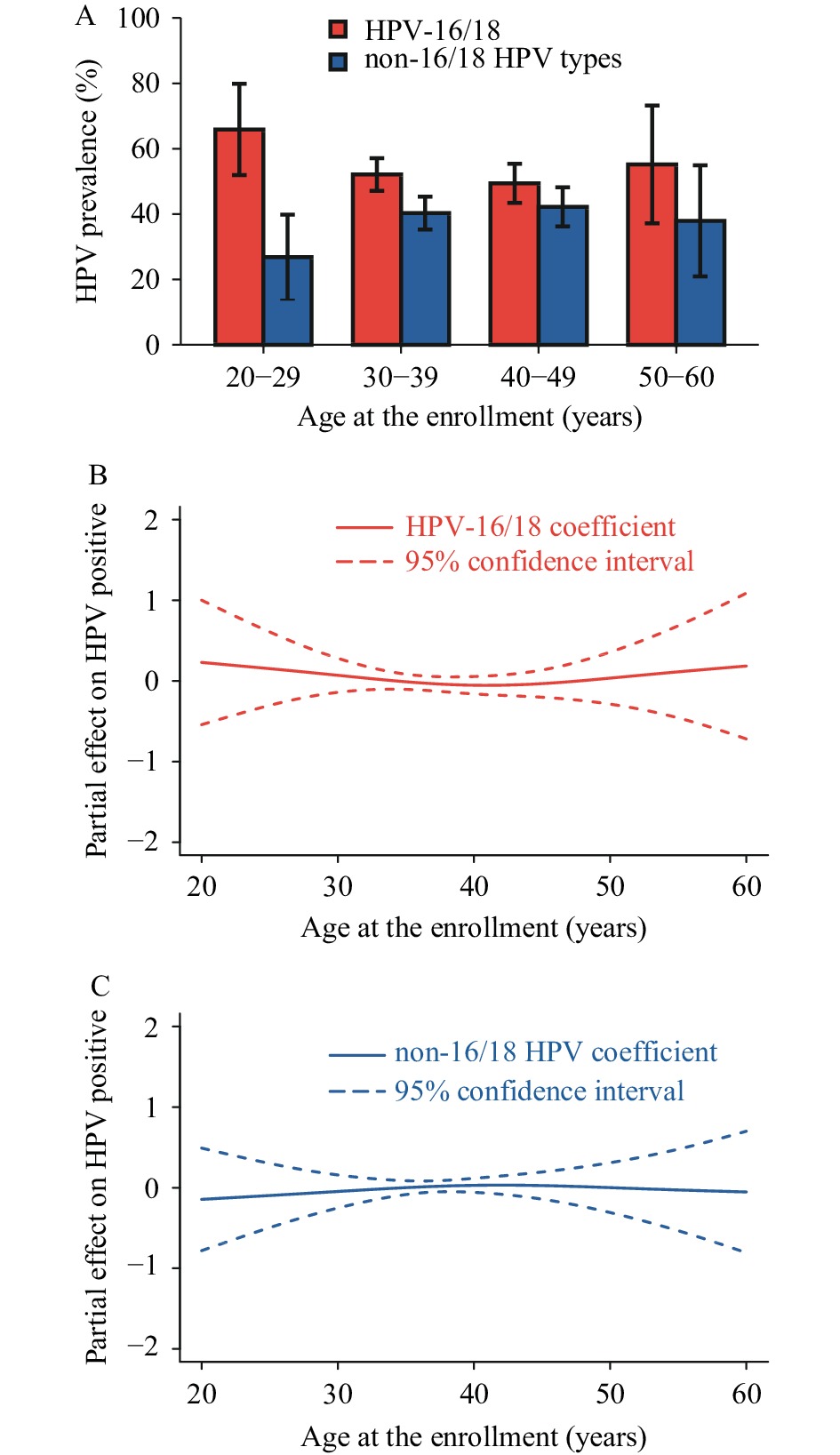
Human papillomavirus (HPV) type-specific strategies play a key role in the prevention of cervical intraepithelial neoplasia (CIN), but evidence on the HPV type-specific prevalence in CIN is limited.
This multicentric study estimates the prevalence of high-risk HPV types in CIN cases and the associations of HPV infection patterns with high-grade CIN in China in 2017–2018.
Population-based prevention strategies should give preference to HPV-16 and 18, and strategies for non-16/18 high-risk HPV are essential for the elimination of cervical cancer.
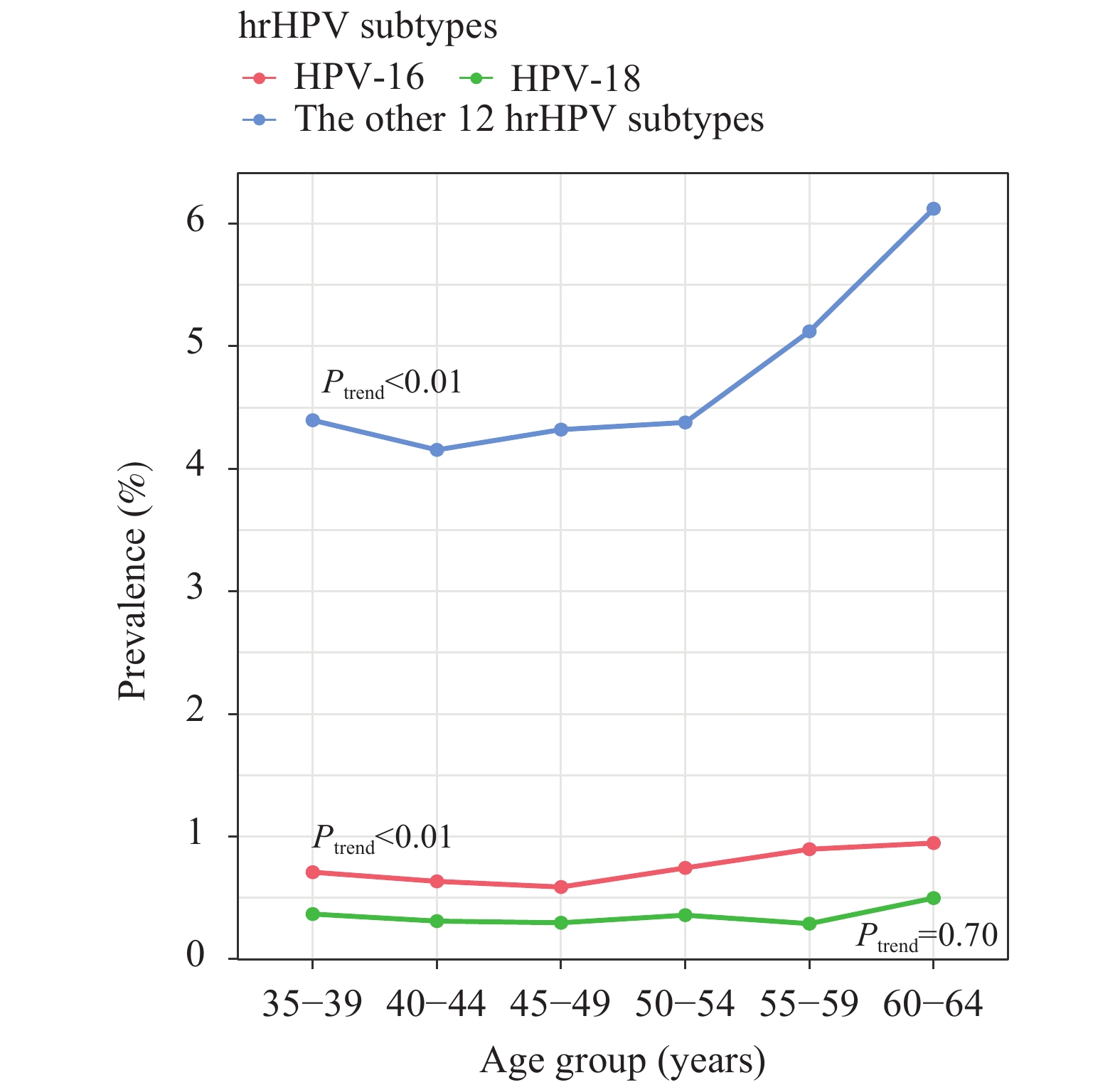
Little is known about the infection pattern for high-risk human papillomavirus (hrHPV) subtypes in rural areas in southern China.
The prevalence of HPV-16, 18, and the other 12 hrHPV subtypes were 0.71%, 0.34%, and 4.50%, respectively, among rural women in Guangzhou. The prevalence of HPV-16 and the other 12 hrHPV subtypes increased with age, but there was no evident age trend for HPV-18 prevalence.
Epidemiological characteristics of hrHPV prevalence in rural Guangzhou should be considered to identify high-risk populations of hrHPV infection and determine follow-up strategies.


 Subscribe for E-mail Alerts
Subscribe for E-mail Alerts CCDC Weekly RSS Feed
CCDC Weekly RSS Feed