2022 Vol. 4, No. 25
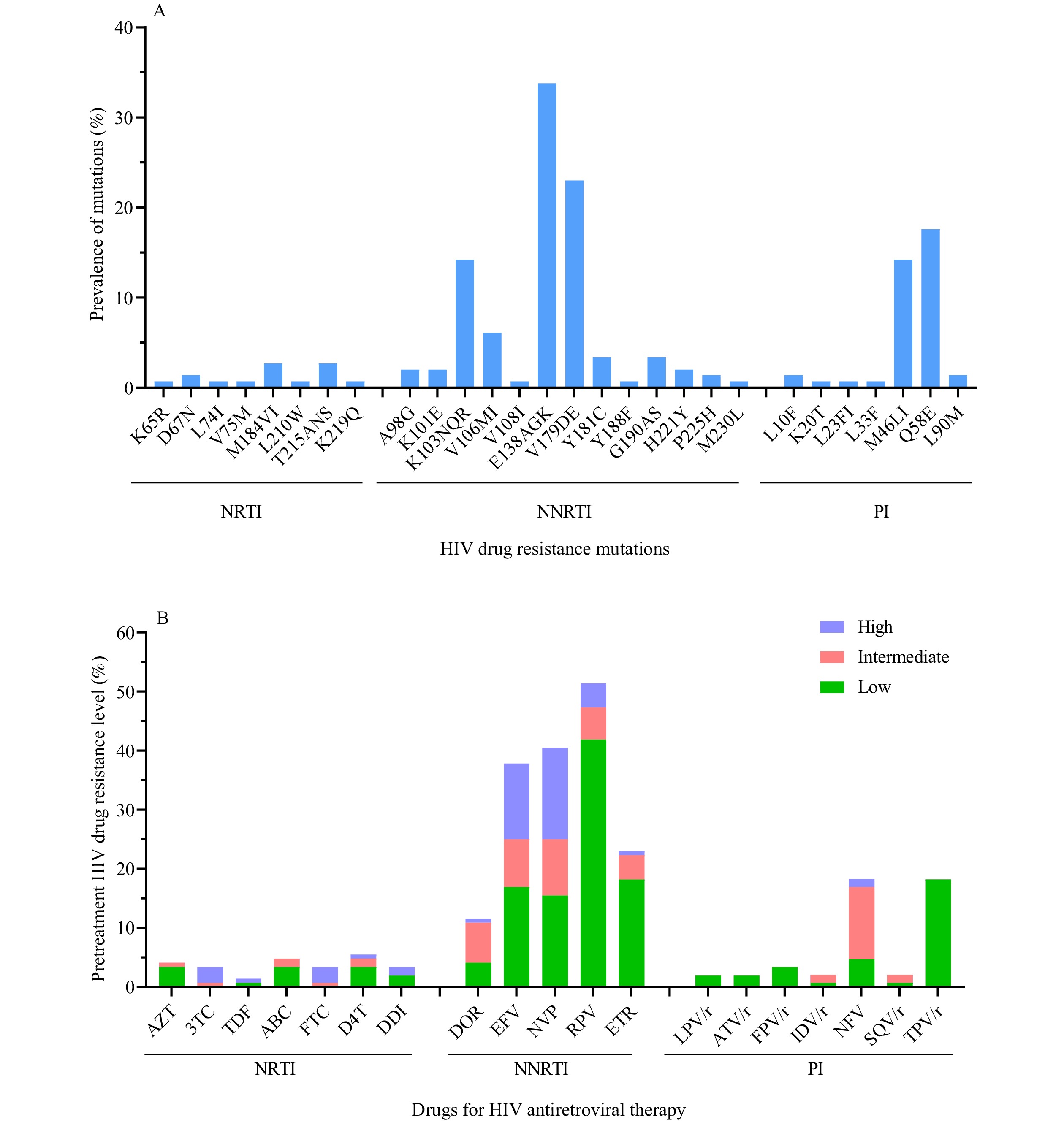
While antiretroviral therapy (ART) has been rapidly scaled-up among the population living with human immunodeficiency virus or acquired immune deficiency syndrome (HIV/AIDS) patients since 2016, pretreatment drug resistance (PDR) has also increased.
PDR has an impact on ART outcomes. After one year of ART, the risk of virological failure in individuals with PDR was found to be 2.3 times higher than that of individuals without PDR. Moreover, patients with PDR to non-nucleoside reverse transcriptase inhibitors (NNRTIs) had an even higher risk of virological failure, with an odds ratio of 2.8 as compared with those without PDR.
PDR is associated with an increased risk of virological failure. It is recommended to regularly implement PDR monitoring in order to provide information to optimize ART regimens and to prevent HIV drug resistance.
Unprotected oral sex carries a risk of the transmission of sexually transmitted infections (STIs), especially if the individual has poor oral health.
Most human immunodeficiency virus (HIV) infected men who have sex with men (MSM) had never used a condom when giving oral sex (89.30%, 718/804) or receiving oral sex (90.32%, 709/785). Among MSM with detectable viral loads who had ever received oral sex without a condom, 40.00% reported ejaculation in their partner’s mouth.
Unprotected oral sex is very common among HIV-infected MSM in China. The public health sectors in China should recommend condom use during oral sex among HIV-infected MSM, especially when in-mouth ejaculation is involved.
Human immunodeficiency virus (HIV) testing is a critical tool in reducing HIV transmission among men who have sex with men (MSM); young MSM frequently use mobile phone applications and participate in social hook-ups.
The prevalence of HIV testing-frequency (≥2) over the whole study period (15 months) was 38.6% among college MSM in Northeast China. MSM with more social contacts, recreational drug use, and prior HIV self-test experience (reported via mobile phone geo-social apps) were more likely to have higher offline HIV testing frequency.
A gay-oriented app provides opportunities for online interventions to promote HIV testing services.
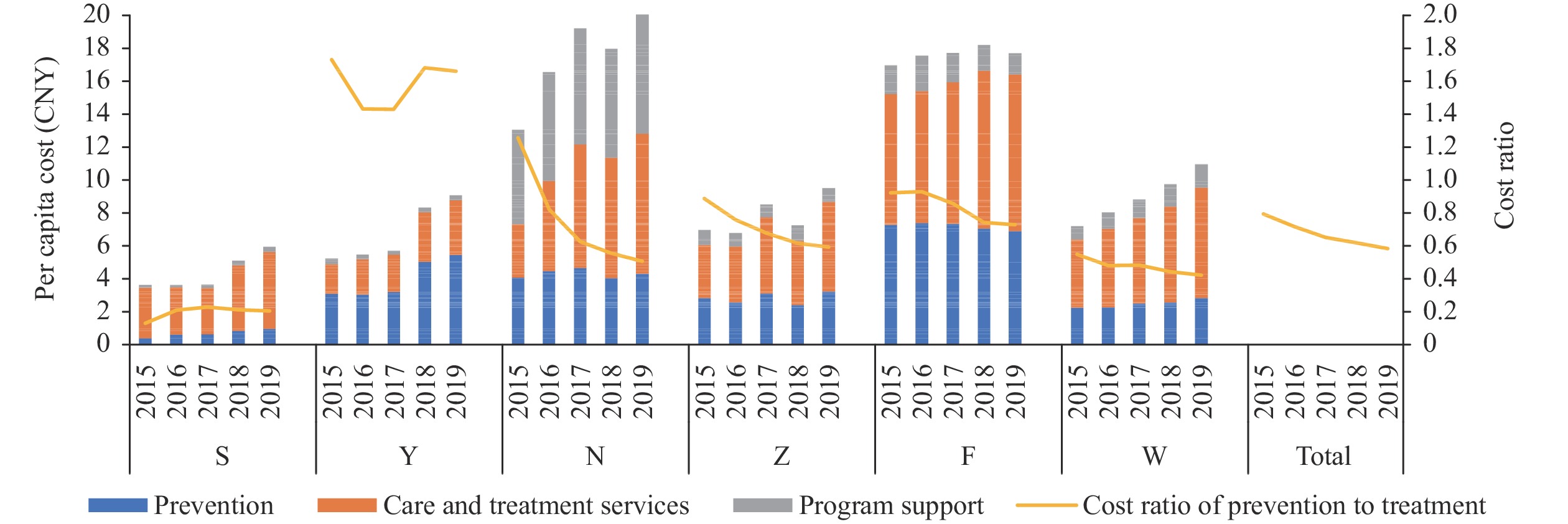
In order to facilitate human immunodeficiency virus (HIV) treatment and prevention, the resource needs for HIV national strategic planning in developing regions were estimated based on Spectrum, the universal HIV cost-effectiveness analysis software.
Based on the theoretical framework of Spectrum, the study developed a cost measurement tool for HIV, and calculated the cost of HIV prevention and control in 6 sampled cities in China during 2015–2019 using the Spectrum model.
From 2015 to 2019, the average annual costs for HIV prevention and control for Shijiazhuang, Yantai, Ningbo, Zhenjiang, Foshan, and Wuxi cities were 46.78, 47.55, 137.49, 24.73, 74.37, and 58.30 million Chinese yuan (CNY), respectively. The per capita costs were 4.37, 6.73, 17.33, 7.77, 17.56, and 8.91 CNY, respectively. In terms of the cost structure, the ratio of preventive intervention funds to therapeutic intervention funds (antiviral treatment) varied in sampled cities.
Developing comprehensive and systematic HIV fund calculation methods can provide a research basis for rational resource allocation in the field of HIV.


 Subscribe for E-mail Alerts
Subscribe for E-mail Alerts CCDC Weekly RSS Feed
CCDC Weekly RSS Feed