-
The human immunodeficiency virus/acquired immunodeficiency syndrome (HIV/AIDS) epidemic in China remains at a low epidemic level nationwide but is highly concentrated in some regions and in some high-risk populations (1). The National HIV Sentinel Surveillance System (HSSS) was established in 1995 in China, but with changes in the HIV epidemic and increasing resources for HIV prevention and control, the development of the HSSS can be divided into 2 stages: active surveillance (1995–1998) and comprehensive surveillance (1999–present). After rapid expansion of national sentinel surveillance in 2010, this system included a nationwide surveillance network including serological and behavioral surveillance from 8 HIV-related populations. After 2010, there were 299 sentinel sites for drug users (DUs) across 30 provincial-level administrative divisions. This study was aimed to analyze serological results among the different types of DUs in HIV sentinel surveillance, for purpose of the providing information and evidence for prevention and scientific intervention to DUs.
Serial cross-sectional surveys were conducted annually among DUs from April to June. The sample size of each HSSS site was approximately 400, though if HIV prevalence within a site exceeded 10%, 250 participants were sampled. Over 60% of DUs were recruited from compulsory detoxification centers with the rest being from the community and methadone maintenance treatment (MMT) clinics. The participants in compulsory detoxification centers were recruited using consecutive sampling, and the participants from MMT clinics were required to have positive urine test results from a recent month before using consecutive sampling. When the participants were recruited from community, snowball sampling could be applied. After providing informed consent, participants completed an anonymous, structured questionnaire which included demographic information, HIV-related behaviors, and serological screening testing of HIV and hepatitis C virus (HCV) conducted by local CDC. Serological testing of HIV and HCV were conducted using the standard protocol and laboratory methods by National Center for AIDS/STD Control and Prevention (NCAIDS).
For both HIV and HCV, initial screening was done by using enzyme-linked immunosorbent assays (ELISA). If the screening result was positive, another test was required using another ELISA. Participants with 2 positive ELISA results in the surveillance system were defined antibody positive. Those who were finally confirmed positive would be referred to treatment and care in local institutions. If patients have been previously confirmed as HIV and/or HCV positive, they were not administered testing via ELISA and given the questionnaires only. Details on the criteria of HSSS have been described elsewhere (2-3). The antibody positive rates were analyzed at the national level annually from 2010 to 2018, and their trends in HIV and HCV antibody positive rates were assessed by the Linear-by-Linear Association test using SPSS software (version 18.0; IBM Corporation).
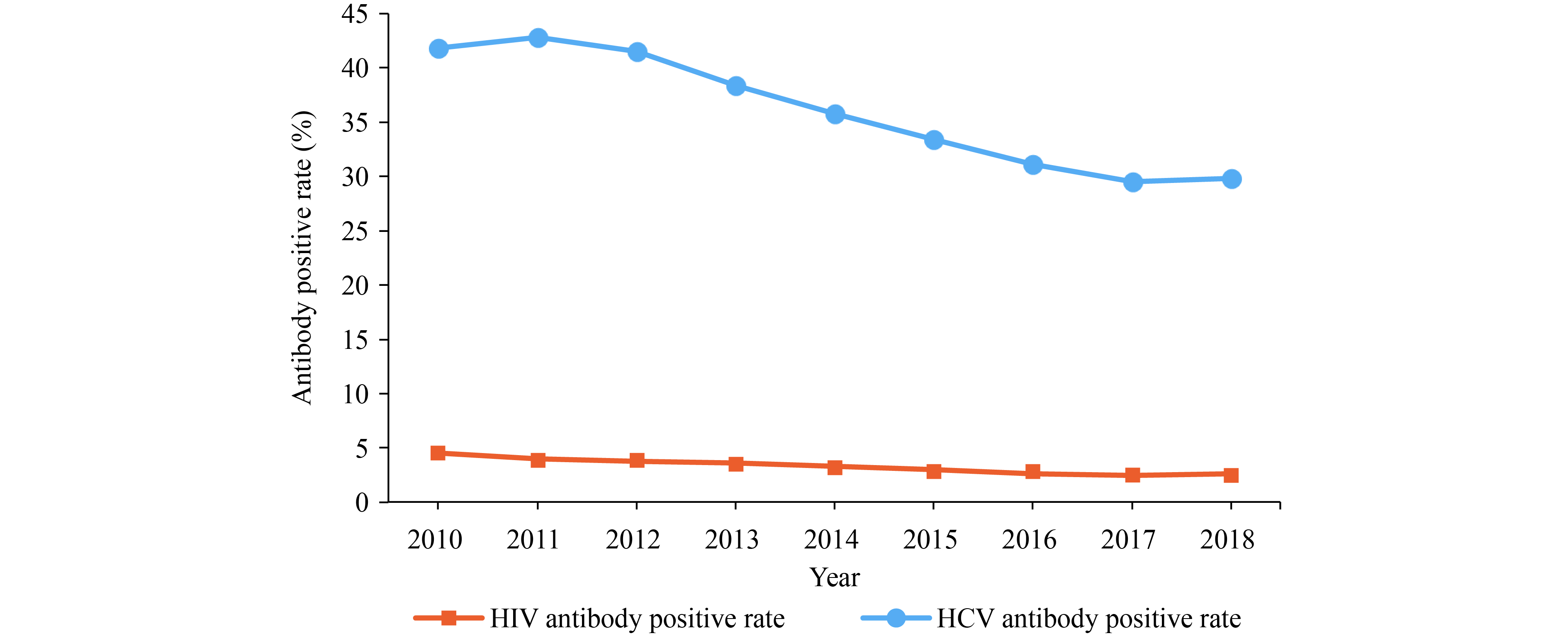
From 2010 to 2018, DUs sentinel surveillance indicated that the HIV antibody positive rate decreased from 4.5% to 2.6% (Linear-by-Linear Association
${\chi ^2}$ =1,354.218, p<0.001) and that the HCV antibody positive rate decreased from 41.8% to 29.8% (Linear-by-Linear Association${\chi ^2}$ =10,220.375, p<0.001) (Figure 1). The proportion of traditional drug users (having used heroin, etc.) decreased from 79.7% in 2010 to 49.3% in 2018, and the proportion of new narcotic users (having used meth, etc.) increased from 14.9% to 42.3% with the proportion of mixed drug users (having used both of two kinds of drugs above) increasing from 5.4% to 8.4%. (Pearson${\chi ^2}$ =59,091.176, p<0.001). During 2010–2018, the HIV antibody positive rate of traditional drug users deceased from 5.4% to 4.3% (Linear-by-Linear Association${\chi ^2}$ =167.657, p<0.001), and the HIV antibody positive rate of new narcotic users fluctuated at level of 0.5% (Linear-by-Linear Association${\chi ^2}$ =0.074, p>0.5) with that of mixed drug users increasing from 1.7% to 3.1% (Linear-by-Linear Association${\chi ^2}$ =35.830, p<0.001) (Figure 2). Between 2010 and 2018, the HCV antibody positive rate of traditional drug users deceased from 47.1% to 44.1% (Linear-by-Linear Association${\chi ^2}$ =748.705, p<0.001), and the HCV antibody positive rate of new narcotic users deceased from 14.7% to 11.5% (Linear-by-Linear Association${\chi ^2}$ =240.490, p<0.001), with that of mixed drug users decreasing from 44.8% to 41.4% (Linear-by-Linear Association${\chi ^2}$ =61.704, p<0.001) (Figure 3).
HTML
-
From 2010 to 2018, the overall HIV and HCV prevalence in DUs both showed decreases (4), and both were relatively stable from 2014 to 2018 at 2.5% and 30%, respectively. The decreases may not only result from decreasing proportion of traditional drug users with decreased HIV and HCV prevalence associated with continuous and effective prevention and comprehensive intervention strategy among injecting traditional drug users (5-7), but also may be related to the increasing proportion of new narcotic users with the lower HIV and HCV prevalence.
The HIV and HCV prevalence of traditional drug users decreased but remains at a relatively high level due to blood transmission. The HIV prevalence of new narcotic users fluctuated around 0.5%, and the HCV prevalence of new narcotic users decreased (from 14.7% to 11.5% between 2010 and 2018), but the overall levels were lower owing to sexual intercourse (8-9). Sentinel surveillance system data showed that the HIV prevalence of participants using both 2 kinds of drugs above increased year by year, while its HCV prevalence had a same level according to the traditional drug users.
In addition, the abuse of new narcotic drugs has become a major problem among drug users in China, especially the abuse of methamphetamine, which accounts for 56.1% of all registered drug users (10). In this study, the proportion of new narcotic users was nearly 50% in recent years, which was consistent with the current pattern of drug use in China (10). Although the proportion of participants using both traditional drugs and new narcotic drugs was less than 10% in sentinel surveillance system, it also showed an increasing trend which was similar to the situation of mixed abuse 2 kinds of drugs above among drug users in China (10).
In summary, HIV and HCV epidemics in DUs were controlled effectively in China during 2010–2018, but HIV and HCV infections were detected in the HSSS every year. Existing strategies and measures mainly target traditional drug users and have successfully reduced HIV transmission through intravenous injection, which needs continued maintenance and potential strengthening in the future. Some existing policies and strategies publicity, education, and interventions require adjustments since new narcotic drug users contributed to DUs HIV infections. The challenge of HIV infection and transmission among drug users abusing both traditional and new narcotic drugs also require more attention. The risk and reasons of transmission need to be evaluated and verified based on analysis of the existing data, combined with further epidemiological survey if necessary, in order to provide scientific evidence for the adjustment of HIV prevention control strategies and intervention measures for drug users.
This study is subject to some limitations. First, the study uses cross-sectional data, which is inherently descriptive and observational. Therefore, the trends described are unable to examine causal relationships. Second, sentinel surveillance data from DUs are based on stratified snowball sampling and convenience sampling and may not be representative of the overall population of DUs in China. Third, the antibody positive rate in sentinel surveillance can represent overall prevalence, which can often be overestimated because it does not account for the results of confirmation testing or RNA testing. Fourth, the recruitment process for this study was led by a mix of China CDC and non-governmental organization (NGO) staff, which may result in some selection bias. Finally, some significant results of the analysis may be due to the large sample size and would not otherwise be meaningful.
-
The authors thank all local public health officers and professional technical staff from local CDCs in the 30 provincial-level administrative divisions who conducted DUs sentinel surveillance surveys.
-
The authors declare no competing interests.
| Citation: |



 Download:
Download:















