-
Influenza A viruses of the H1N1 and H3N2 subtypes and influenza B viruses of the Yamagata and Victoria lineages cause annual epidemics in human populations with spikes in circulation during the winter months in the Northern and Southern hemispheres, and year-round circulation in tropical and subtropical climates.
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) is a novel coronavirus that emerged in December 2019 and spread so rapidly around the world that the World Health Organization (WHO) declared a pandemic on March 11, 2020 (1). As of November 23, 2021, more than 258 million cases of SARS-CoV-2 had been reported with more than 5.1 million fatalities (2).
With the rapid spread of SARS-CoV-2 around the world, the rate of influenza virus detection declined dramatically (3-6). WHO Influenza Update No. 376 (7) reported that of 145,068 specimens tested from August 17 to 30, 2020, only 34 were positive for influenza virus (0.02%). During a similar time period in 2019, 4,097 of 57,132 specimens (i.e., 7.2%) were positive for influenza viruses (8). Similarly, of 200,863 specimens tested from December 21, 2020 through January 3, 2021, only 409 were positive (0.2%) (9) while between December 23, 2019 and January 5, 2020, 44,847 of 174,604 specimens were positive (25.7%) (10).
Several hypotheses have been proposed to explain the substantial decline in influenza virus detection rates. First and foremost, non-pharmaceutical intervention strategies including social distancing; travel restrictions; closure of schools, universities, and many public and commercial offices; mask wearing; and improved hand hygiene may have curbed the spread of influenza viruses. In addition, viral interference, whereby innate immune responses to a viral infection can affect infection by a second virus (11-14) have been discussed as a potential mechanism that might explain the low rates of influenza virus circulation in human populations during the SARS-CoV-2 pandemic. However, several studies have demonstrated that influenza viruses can replicate in animals or cells co- or sequentially infected with SARS-CoV-2 (15-17), suggesting that viral interference may not be the major reason for the low influenza virus detection rate during the SARS-CoV-2 pandemic. Interestingly, the decline in detection rates differs among human respiratory viruses. Human coronaviruses, parainfluenza viruses, human metapneumoviruses, respiratory syncytial virus, and adenoviruses have all been detected at very low rates since the outbreak of the SARS-CoV-2 pandemic, whereas rhinoviruses have been detected more frequently (4-5,18), perhaps because of their lower sensitivity to alcohol and detergents compared to other enveloped human respiratory viruses. These findings lead to interesting questions about the similarities and differences among human respiratory viruses regarding their transmission mode and the most effective mitigation strategies.
Many of the influenza viruses isolated in 2020 and 2021 originate from the (sub)tropical regions of the world, where the year-round circulation of influenza viruses (believed to be a consequence of climate and behavioral factors) may have supported low-level influenza virus transmission in communities during the SARS-CoV-2 pandemic. Approaching the influenza virus season in the Northern hemisphere, combined with less restrictive non-pharmaceutical interventions in parts of the world due to increasing SARS-CoV-2 vaccination rates, it will be interesting to see whether influenza viruses make a comeback as major human respiratory pathogens. The latest WHO Influenza Update (19) showed that of 307,999 specimens tested worldwide, 2,199 were positive for influenza viruses, resulting in a detection rate of 0.7%. While this worldwide detection rate is still much lower than prior to the SARS-CoV-2 pandemic, it may suggest increasing influenza virus activity compared to 2020. In particular, parts of Asia (including India and Nepal) have recently experienced increased influenza activity with the number of influenza virus-positive specimens reaching about 50% of the numbers reported before the pandemic (Figure 1); moreover, China has experienced low levels of B/Victoria virus circulation in 2021 (Figure 1).
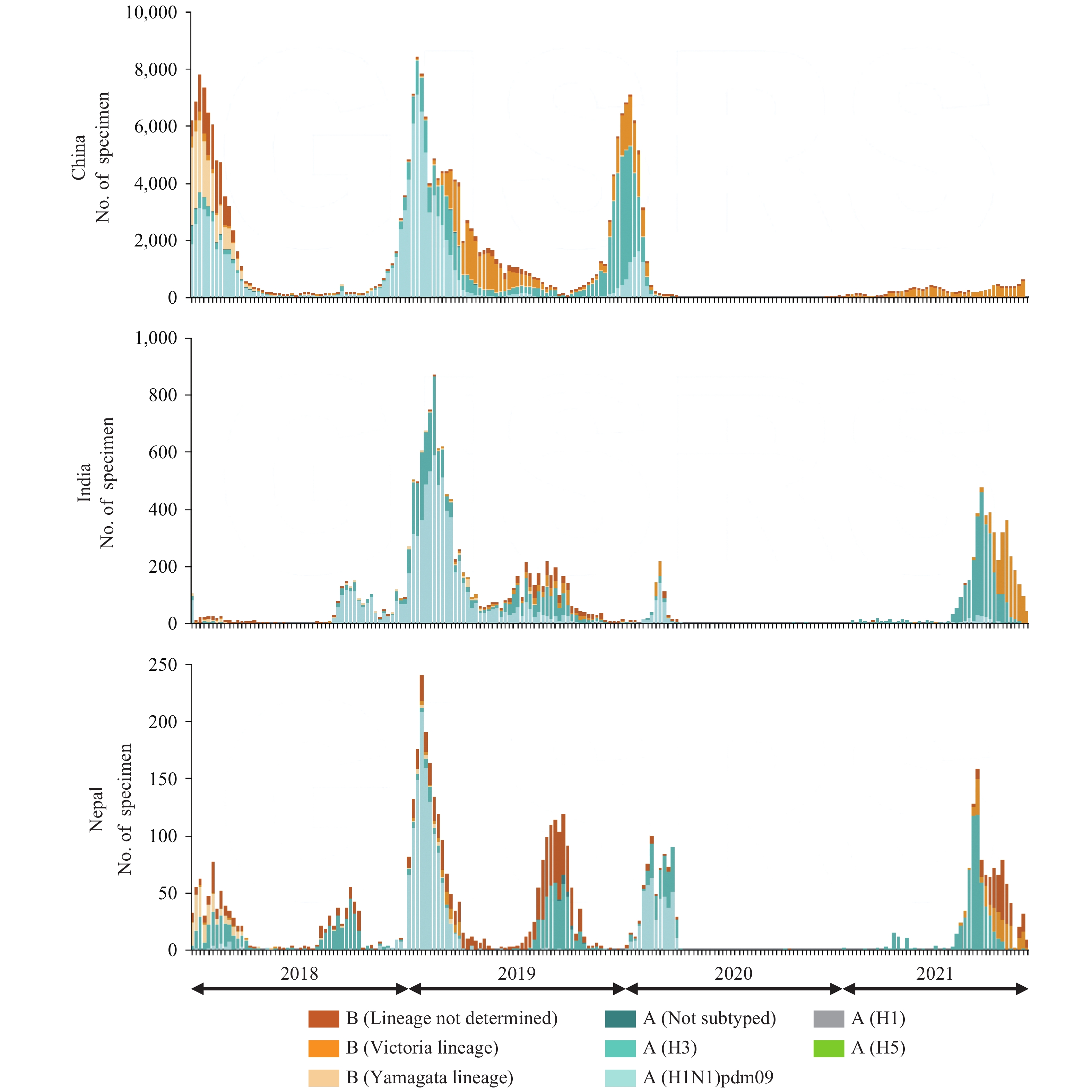 Figure 1.
Figure 1.Number of influenza virus-positive samples since 2018 in China, India, and Nepal. Figure generated from (20).
The massive reduction in the number of circulating human influenza viruses likely created a substantial genetic bottleneck. In fact, the influenza A and B viruses isolated in 2020 and 2021 fall into a limited number of (sub)clades, while other (sub)clades have virtually disappeared, although viruses of these (sub)clades may still be circulating at low levels. Most noticeably, influenza B viruses of the Yamagata lineage have been detected at very low levels; for example, of 1,176 influenza B viruses reported in the last WHO Influenza Update (19), only one belonged to the Yamagata lineage. Currently, it is not clear why certain influenza virus (sub)lineages have declined more than others during the SARS-CoV-2 pandemic. Several factors including population immunity, viral fitness, and the extent of non- pharmaceutical interventions in the areas of virus circulation may have contributed.
In summary, we are currently experiencing an extraordinary event in human influenza virus epidemiology and evolution during which the virus has experienced extreme pressure that may result in major genetic bottlenecks that could shape influenza virus evolution for years to come. With the expected comeback of human influenza virus infections in the ensuing years, which may be fueled by a waning of immune responses in previously exposed people and an increasing number of infants and toddlers who are naïve to influenza viruses, much can be learned about the evolution and spread of influenza viruses in humans.
-
Susan Watson.
HTML
| Citation: |




 Download:
Download:




