2022 Vol. 4, No. 52
Numerous ecological and laboratory studies suggest face masks are an effective non-pharmaceutical intervention for reducing the spread of coronavirus disease 2019 (COVID-19), but cannot otherwise assess individual-level effects.
Using a prospective cohort of individuals enrolled in a participatory, syndromic surveillance tool prior to the first case of COVID-19 in the United States, we present a novel longitudinal assessment of the effectiveness of face masks.
Our analysis demonstrates an association between self-reported mask-wearing behavior and lower individual risk of syndromic COVID-19-like illness while adjusting for confounders at the individual level. Our results also highlight the dual utility of participatory syndromic surveillance systems as both disease trend monitors and tools that can aid in understanding the effectiveness of personal protective measures.
During the coronavirus disease 2019 (COVID-19) pandemic, tremendous efforts have been made in countries to suppress epidemic peaks and strengthen hospital services to avoid hospital strain and ultimately reduce the risk of death from COVID-19. However, there is limited empirical evidence that hospital strain increases COVID-19 deaths.
We found the risk of death from COVID-19 was linearly associated with the number of patients currently in hospitals, a measure of hospital strain, before the Omicron period. This risk could be increased by a maximum of 188.0%.
These findings suggest that any (additional) effort to reduce hospital strain would be beneficial during early large COVID-19 outbreaks and possibly also others alike. During an Omicron outbreak, vigilance remains necessary to prevent excess deaths caused by hospital strain as happened in Hong Kong Special Administrative Region, China.
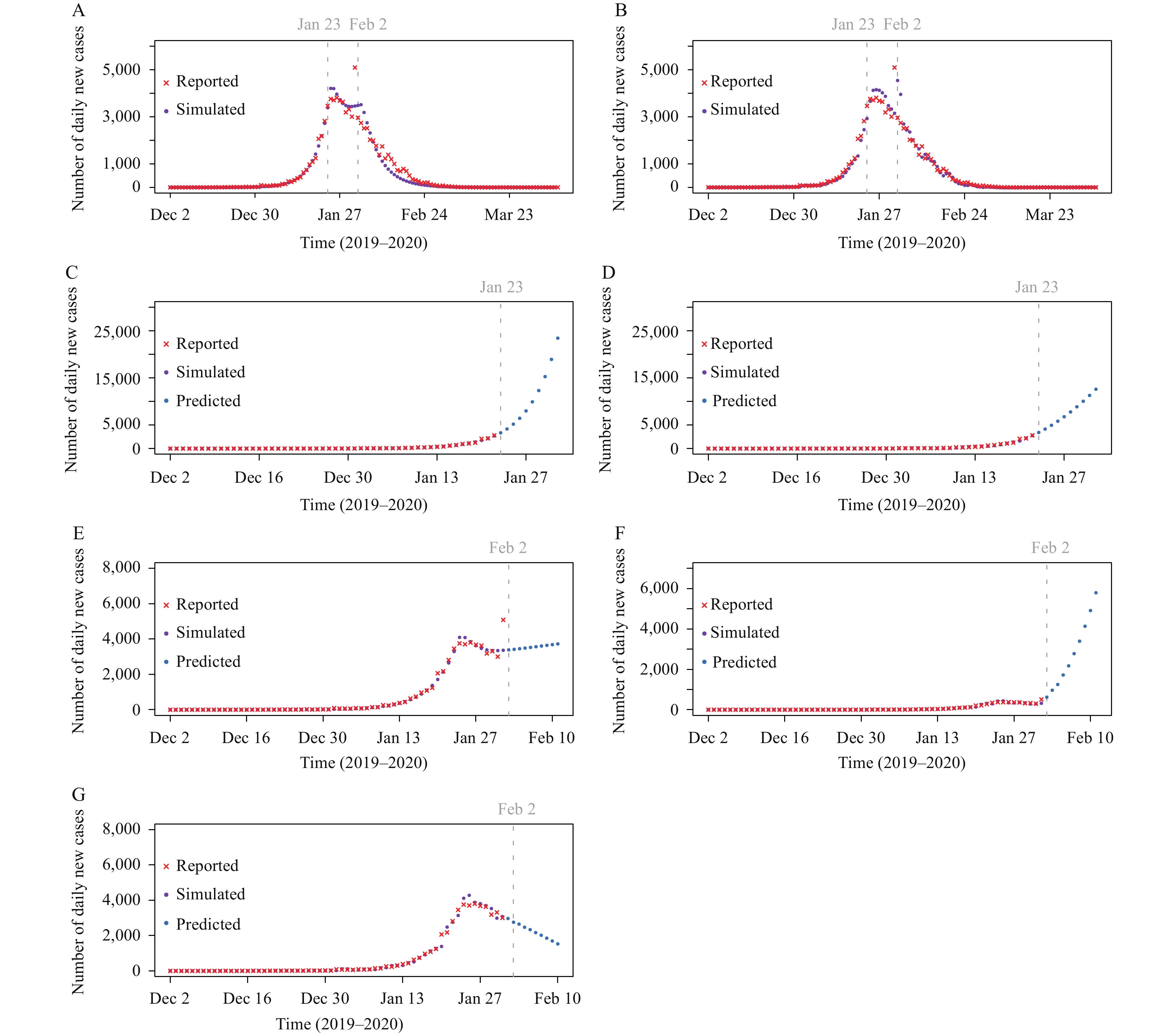
To compare the performance between the compartment model and the autoregressive integrated moving average (ARIMA) model that were applied to the prediction of new infections during the coronavirus disease 2019 (COVID-19) epidemic.
The compartment model and the ARIMA model were established based on the daily cases of new infection reported in China from December 2, 2019 to April 8, 2020. The goodness of fit of the two models was compared using the coefficient of determination (R2).
The compartment model predicts that the number of new cases without a cordon sanitaire, i.e., a restriction of mobility to prevent spread of disease, will increase exponentially over 10 days starting from January 23, 2020, while the ARIMA model shows a linear increase. The calculated R2 values of the two models without cordon sanitaire were 0.990 and 0.981. The prediction results of the ARIMA model after February 2, 2020 have a large deviation. The R2 values of complete transmission process fit of the epidemic for the 2 models were 0.964 and 0.933, respectively.
The two models fit well at different stages of the epidemic. The predictions of compartment model were more in line with highly contagious transmission characteristics of COVID-19. The accuracy of recent historical data had a large impact on the predictions of the ARIMA model as compared to those of the compartment model.



 Subscribe for E-mail Alerts
Subscribe for E-mail Alerts CCDC Weekly RSS Feed
CCDC Weekly RSS Feed